Mental models for handling difficult situations in clinical practice
There may be instances in clinical practice where a wide variety of difficult conversations take place. These difficult interactions may result from differences between the patient's and the doctor's expectations, perceptions, and/or communication.1
Few studies have found that up to 15% of clinical encounters are experienced as difficult by clinicians.2

Following can be the situations that may lead to a difficult situation:1
- Informing about the death of a patient
- Informing about a diagnosis with a poor prognosis
- Informing about an unsuccessful surgery
- Informing about the additional expenses a patient might have to incur
- Informing about a chronic disease without any cure
- Informing about a potential handicap patient may have to bear with
- Long waiting times in the clinic
- Consecutive cancellations or delayed investigations
- Lack of resources in terms of staffing
Factors contributing to a difficult situation:1
A couple of subsets that can be the factors leading to a difficult situation are the patients and the healthcare system. A few reasons which can be the triggering factor ultimately leading to an unpleasant or unwanted situation are given below:

Potential implications of a difficult situation:1
The aftereffects of a difficult or unpleasant situation can also be divided into the subsets: patients and the healthcare system:

Techniques to manage a difficult situation in clinical practice:3
Understanding the reasons behind tough encounters and employing coping mechanisms can help both patients and doctors come to an agreeable conclusion during a consultation. A few mental models suggested below might prove helpful.

Tips to prevent a difficult situation in the clinic:
The first step in addressing the problem is realizing that it is a challenging consultation. Before diagnosing and treating the patient's "illness," the interactional "difficulty" may need to be identified and managed.1
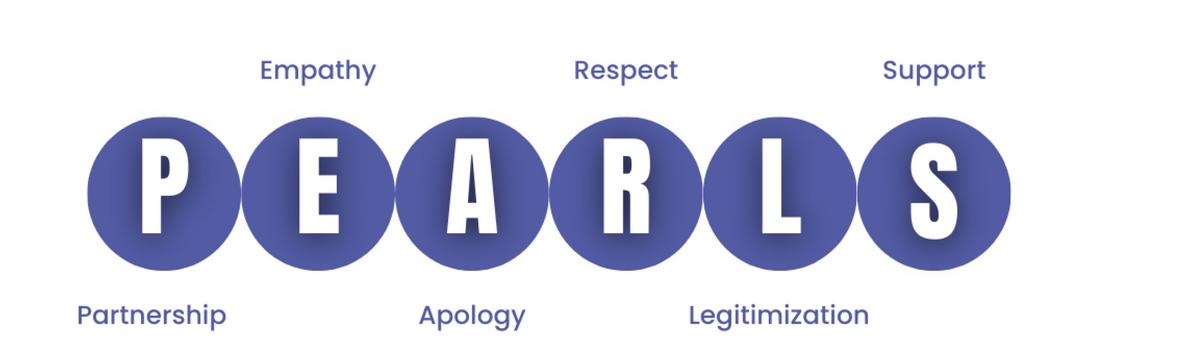
A simple acronym, “PEARLS” which has been supported by John Hopkins Medicine can be followed while communicating with patients which might help in avoiding a difficult situation:4
The hospital needs to be ready to deal with and diffuse the situation if, in the worst event, the difficult situation cannot be controlled by the above-mentioned techniques and escalates into a violent one.5
- An SOS button or a speed dial on the mobiles of the doctors to alert the security department. Round-the-clock security team to be present in the hospital
- A centralized and well-equipped CCTV camera system for monitoring and quick response
- Display of legislation protecting doctors in every hospital and police station
- The contact details of the closest police station should be available easily to the hospital staff
Conclusion:6
Preparation is essential when it comes to delivering difficult-to-hear information to patients. Review the clinical situation, give yourself enough time and solitude, and be aware of the listeners. Determine what the patient already knows or believes about the situation at the outset of the session and how much more information he or she needs. Directly inform the patient and others around of the news, giving them enough time to comprehend it and experience their emotions. After breaking the news, talk about the consequences, give further resources, decide on the next steps, wrap up the conversation, and make sure to make follow-up arrangements.
It will help to avert problematic clinical interactions if you are aware of the contributing variables and are ready to handle them. But the positive impact that effective interpersonal communication skills can have should not be undervalued.
References
- Hardavella G, Aamli-Gaagnat A, Frille A, Saad N, Niculescu A, Powell P. Top tips to deal with challenging situations: doctor–patient interactions. Breathe [Internet]. 2017 Jun;13(2):129–35. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5467659/
- Hinchey SA, Jackson JL. A Cohort Study Assessing Difficult Patient Encounters in a Walk-In Primary Care Clinic, Predictors and Outcomes. Journal of General Internal Medicine. 2011 Jan 25;26(6):588–94.
- Davies M. Managing challenging interactions with patients. BMJ [Internet]. 2013 Jul 31;f4673. Available from: https://www.bmj.com/content/347/bmj.f4673
- Defusing Difficult Situations [Internet]. www.hopkinsmedicine.org. Available from: https://www.hopkinsmedicine.org/office-of-johns-hopkins-physicians/best-practice-news/defusing-difficult-situations
- MECHANISM TO PREVENT VIOLENCE AGAINST DOCTORS [Internet]. pib.gov.in. [cited 2023 Feb 9]. Available from: https://pib.gov.in/Pressreleaseshare.aspx?PRID=1806206
- Hull SK, Broquet K. How to Manage Difficult Patient Encounters. Family Practice Management [Internet]. 2007 Jun 1;14(6):30–4. Available from: https://www.aafp.org/pubs/fpm/issues/2007/0600/p30.html



