APSC Consensus Recommendations on Dyslipidemia

The Asian Pacific Society of Cardiology (APSC) consensus recommendations for management of dyslipidemia.
Koh N, Ference BA, Nicholls SJ, Navar AM, Chew DP, Kostner K, et al. Eur Cardiol. 2021;16:e54.
Key Takeaway
The APSC consensus recommendations tackled contemporary issues in the management of dyslipidemia, FH and Lp(a) in the Asia-Pacific region based on most updated evidence.
- These included 14 recommendations for
- Assessment of patients with chronic coronary syndrome (CCS)
- LDL-C treatment targets
- Therapy for high-risk and very high-risk CCS
- Criteria for identification, diagnosis, and cascade screening of suspected FH
- Measurement of Lp(a) in specific populations
- The recommendations by APSC intend to guide assessment and treatment of dyslipidemia to facilitate improved screening, early diagnosis, and treatment.
- Dyslipidemia should be managed on an individual basis.
- The clinicians should be conscious of the challenges that may limit the applicability of these consensus recommendations
- The recommendations should not substitute clinical judgement.
Why This Matters
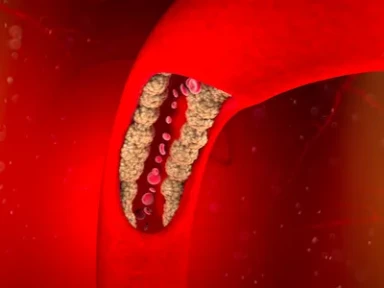
- The increasing prevalence of dyslipidemia in the Asia Pacific is associated with dietary changes and decreasing physical activity.
- While there has been substantial progress in dyslipidemia therapy, its management in the Asia-Pacific region is challenged by limitations in awareness, adherence, and healthcare costs.
- A unified approach for the management of dyslipidemia is needed.
Consensus Recommendations
6 Consensus Recommendations - Dyslipidemia
- Patients with CCS should be assessed according to the Coronary–Vascular–Disease system (APSC CCS consensus recommendations) and categorized as having high-risk CCS (one risk factor) or very-high-risk CCS (>1 risk factor) (level of evidence, low; consensus, 96.3% agree)
- High-intensity statins are recommended for all patients with clinically manifest CCS, regardless of risk (level of evidence, moderate; consensus, 88.9% agree)
- LDL-C treatment targets for high-risk CCS: Reduction from baseline LDL-C of ≥50% and achieving an on-treatment level of at least <1.8 mmol/l (level of evidence, low; consensus, 96.3% agree)
- LDL-C treatment targets for very high-risk CCS: Reduction from baseline LDL-C of ≥50% and achieving an on-treatment level of at least <1.4 mmol/l (level of evidence, low; consensus, 96.3% agree)
- For high-risk CCS on maximally tolerated statins: Ezetimibe and/or a PCSK9i may be added for those who do not achieve target (level of evidence, moderate; consensus, 100% agree)
- For very-high-risk CCS:
- Upfront initiation of combination therapy with high-intensity statins and ezetimibe may be considered
- A PCSK9i may be added for those who do not achieve target within 4 weeks of initial therapy (level of evidence, moderate; consensus, 96.3% agree)
5 Consensus Recommendations - Familial Hypercholesterolemia
- Consideration of FH should be in people with:
(1) Severely elevated LDL-C (in adults, >4.9 mmol/l; in children [aged ≤19 years], >3.9 mmol/l) (2) LDL-C of >2.6 mmol/l while adherent to a high-intensity statin (3) Premature ASCVD (age: men, <55 years; women, <60 years) (4) Elevated LDL-C (in adults >4.1 mmol/l) and a first-degree relative with premature CVD (5) A first-degree relative with FH, tendon xanthoma or arcus cornealis (level of evidence, low; consensus, 100% agree) - Clinical criteria can be used to identify and diagnose suspected FH
- Choice of criteria may vary across and within countries) (level of evidence, low; consensus, 96.3% agree)
- Confirmation of FH via genetic testing is not necessary for treatment initiation but may be, for diagnostic confirmation and cascade screening to identify family members with FH (level of evidence, low; consensus, 100% agree)
- Once an index case is diagnosed, family cascade screening (lipid profile) is recommended (level of evidence, low; consensus, 96.3% agree)
- Patients with FH and ASCVD or another major CV risk factor are considered as very high risk
- All other patients with FH are considered as high risk
- These patients should be treated with LLTs in accordance with their risk profile (level of evidence, low; consensus, 96.3% agree)
3 Consensus Recommendations – Lipoprotein(a)
- Resources permitting Lp(a) measurement should be performed at least once in each adult person’s lifetime, especially those with family history of premature ASCVD
- Those with very high inherited Lp(a) levels >430 nmol/l (>180 mg/dl) may have a lifetime ASCVD risk equivalent to the risk associated with heterozygous FH (level of evidence, low; consensus, 92.6% agree)
- Consideration of Lp(a) measurement in selected patients with family history of premature CVD (level of evidence, low; consensus, 92.6% agree)
- As Lp(a) is a risk enhancer, measurement may be considered for between high- and very-high risk groups (level of evidence, low; consensus, 92.6% agree)
APSC, Asian Pacific Society of Cardiology; ASCVD, Atherosclerotic Cardiovascular Disease; CCS, Chronic Coronary Syndrome; CV, Cardiovascular; CVD, Cardiovascular Disease; FH, Familial Hypercholesterolemia; LDL-C, Low-Density Lipoprotein-Cholesterol; LLTs, Lipid-Lowering Therapies; Lp(a), Lipoprotein(a); PCSK9i, Proprotein Convertase Subtilisin/Kexin type 9 inhibitor.
- Koh N, Ference BA, Nicholls SJ, Navar AM, Chew DP, Kostner K, et al. Asian Pacific Society of Cardiology consensus recommendations on dyslipidaemia. Eur Cardiol. 2021;16:e54. doi: 10.15420/ecr.2021.36. PMID: 35024056.

-from-the-SAFEHEART-registry.webp/jcr:content/Clinical%20practice%20experience%20in%20patients%20with%20familial%20hypercholesterolemia%20(FH)%20from%20the%20SAFEHEART%20registry.webp)