Importance of lipid registries in cardiovascular prevention
Key Takeaway
In clinical practice, there exist a gap between lipid guidelines and lipid management - use of combination therapy and improving patient adherence should be prioritized
- Only half of the patients with CVD received high-intensity statins
- Less than half attained the LDL-C goal in secondary prevention
Major reasons for insufficient therapy:
- Side effects of LLT
- Poor adherence to medication regimens
- Low use of combination therapies by physicians
Why This Matters
- Extrapolating data from clinical trials of specifically selected populations to usual care in clinical practice is limited.
- Lipid registry-based research is an important tool for evaluating current lipid management in patients at risk of CVD.
Key Highlights
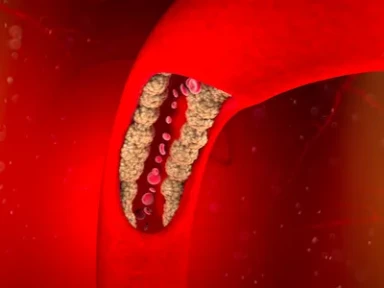
Various clinical guidelines recommend LLTs for ASCVD prevention
- CV event risk remains in high-risk patients with multiple risk factors/established ASCVD
- It is important to quantify accurately if these high-risk patients are receiving guideline-recommended LLTs and attaining optimal recommended LDL-C levels in routine clinicalpractice.
Occurrence of ASCVD events§ was assessed between hospital discharge for each patient’s index AMI¶and their first fill for a PCSK9i.
| Registries of Lipid management |
Study Findings |
| Euroaspire v |
|
| Da Vinci |
|
| Dysis II |
|
| Gould |
|
| Palm |
|
Barriers to lipid management
Majority of secondary patients receive inadequate LLT
- Guideline-recommended LDL-C goal is not achieved with monotherapy,especially in high-risk patients
Data highlight the importance of combination therapies and intensive LLT regimens including greater utilization of non-statin LLTs
Poor adherence of both patients and physicians to LLTs is associated with increased variability in LDL-C levels
- Non-statin LLTs (ezetimibe/PCSK9 inhibitor) may be useful for these issues
Tailored interventions*based on each patient’s requirements are important
*Such as optimal treatment, simple regimen, education, regular monitoring, and feedback during their treatments
ACS, Acute Coronary Syndrome; ASCVD, Atherosclerotic Cardiovascular Disease; CV, Cardiovascular; CVD, Cardiovascular Disease; DA VINCI; EU-Wide Cross-Sectional Observational Study of Lipid-Modifying Therapy Use in Secondary and Primary Care; DYS IS II, Dyslipidemia International Study II; EUROASPIRE, European Action on Secondary Prevention Through Intervention to Reduce Events; GOULD, Getting to an Improved Understanding of Low-Density Lipoprotein Cholesterol and Dyslipidemia Management; LDL-C, low-density lipoprotein cholesterol; LLT, Lipid-lowering Therapy; PALM, Patient and Provider Assessment of Lipid Management; PCSK9, Proprotein Convertase Subtilisin/Kexin type 9.
- Nishikido T, Ray KK. The power of lipid registries for cardiovascular disease prevention. Curr Opin Lipidol. 2021;32(6):342-348. doi: 10.1097/MOL.0000000000000783. PMID: 34561312.(Nishikido T, et al. Curr Opin Lipidol. 2021;32(6):342-348.



-from-the-SAFEHEART-registry.webp/jcr:content/Clinical%20practice%20experience%20in%20patients%20with%20familial%20hypercholesterolemia%20(FH)%20from%20the%20SAFEHEART%20registry.webp)