PCSK9 Inhibitors in Real World Practice

Effectiveness and safety of PCSK9 inhibitors in Czech real-world practice.
Proprotein convertase subtilisin/kexin type 9 inhibitors (PCSK9i) were effective and well-tolerated, with sustained effects, comparable to those in randomized studies.
Key Takeaway
- PCSK9i were effective in statin-intolerant patients, as significantly lower levels of low-density lipoprotein-cholesterol (LDL-C) were seen within 12 weeks.
- Target LDL-C levels were attained by 35.9% of patients in primary atherosclerotic cardiovascular disease (ASCVD) prevention and 65.7% of those in secondary ASCVD prevention at 1 year after therapy initiation.
Why This Matters
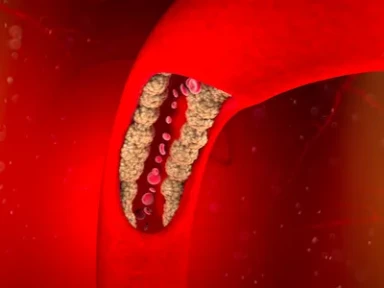
- In patients with ASCVD with insufficient response or intolerant to traditional LDL-C-lowering therapies, PCSK9i can be beneficial.
- The extent to which the outcomes of therapy with PCSK9i in Czech real-world practice was comparable with those reported by large, randomized studies involving Czech patients was unknown.
Study Design
- The effect of PCSK9i therapy was assessed in the entire study population (N = 314; men = 44%; mean age = 63 years) in a Prague-based center of preventive cardiology between 31 July 2018 and 30 September 2020, including in the following subgroups of patients:
- With familial hypercholesterolemia (FH, 65%) vs. without FH, with LDL-C levels ≥4 mmol/L despite maximum tolerated dose (MTD) of statin
- Ezetimibe was given as an add-on, except if LDL-C levels were >50% than target if statin-naïve, or >20% if on statin at MTD
- With FH in primary (69%) or secondary (31%) ASCVD prevention, with LDL-C levels ≥3 mmol/L, despite lipid-lowering therapy at MTD
- Without FH in secondary ASCVD prevention (n = 107)
- On PCSK9i monotherapy alone vs. PCSK9i in combination with a statin
- With familial hypercholesterolemia (FH, 65%) vs. without FH, with LDL-C levels ≥4 mmol/L despite maximum tolerated dose (MTD) of statin
- Potential differences in the effect and tolerability of alirocumab (75 mg or 150 mg; n = 113) and evolocumab (140 mg; n = 156) were also assessed.
- Primary endpoints: Change in LDL-C, total cholesterol (TC), lipoprotein (a) Lp(a), apolipoprotein B (apoB), high-density lipoprotein-cholesterol (HDL-C), and triglycerides (Tg) at 12 and 24 weeks, and 1 and 2 years after initiation of therapy with PCSK9i
- Secondary endpoints: Impact on glucose metabolism
Key Results
Effect on lipid parameters
- Changes in LDL-C levels: There was a significant reduction at 12 weeks (−59.4%) that continued to persist at 2 years (−62.6%)
- Changes in TC levels: There was a significant reduction at 12 weeks (decrease by 41.7%) and at 2 years (decrease by 43.9%)
- Changes in Lp(a) levels: There was a reduction at 12 weeks (−25.4%) and a further reduction at 24 weeks (−35.5%)
- Changes in apoB levels: There was a significant reduction at 12 weeks (54.2%) and at 2 years (58.1%)
- Changes in HDL-C levels: There was a slight increase at 12 weeks (4%) and at 2 years (5.6%)
- Changes in Tg levels: There was a significant reduction at 2 years (−30.3%), with levels reaching targets set by the 2019 ESC/EAS guidelines
Effect on glucose parameters
- Glucose metabolism was not affected by PCSK9i therapy
Effect on patients with and without FH
- Dynamics of decrease after therapy initiation were similar, with a decrease in LDL-C levels by 56.7% and 61.8% at 12 and 24 weeks in patients with FH compared to 67.4% and 68.8% in patients without FH, respectively
- At 2 years, significantly lower LDL-C levels were observed in both patients with FH (−63.5%) and those without FH (−62.3%)
Effect on patients with primary and secondary ASCVD prevention
- Dynamics of decrease after therapy initiation were similar, with a decrease in LDL-C levels by 55.7% and 61.5% at 12 and 24 weeks in patients in primary prevention, and by 63.9% and 66.3% in those in secondary prevention
- At 2 years, significantly lower LDL-C levels were observed in both patients in primary (−61.7%) and secondary (−64.2%) prevention
Effect on patients tolerant vs intolerant to statins
- By week 12, LDL-C levels in patients on maximum statin dose decreased by 65.2% compared to 55% in those not on statin therapy
- At 2 years, significant differences in LDL-C levels were seen between patients on maximum statin dose vs those who were statin-intolerant (64% vs 59.3%)
Effect on patients treated with alirocumab vs evolocumab
- By week 12, LDL-C levels in patients on alirocumab decreased by 55.5% compared to 66.1% in patients on evolocumab
- At 2 years, significant differences in LDL-C levels were seen (64.7% vs 61%) Correlation between baseline LDL-C levels and their decrease relative to therapy
Correlation between baseline LDL-C levels and their decrease relative to therapy
- Moderately strong inverse correlation (Pearson’s r = −0.7147) was seen
Effect on safety
- Side effects were reported by 9% of patients (alirocumab-related: 14; evolocumab-related: 16); 15 patients withdrew due to side effects
- Flu-like syndrome was more frequent (n = 13), followed by pain at injection site (n = 5), myalgia (n = 5), and gastrointestinal intolerance (n = 3)
Limitations
- Patients were enrolled only from a single center and those not meeting the reimbursement criteria and self-payers were not included.
- Cardiovascular effects of PCSK9i were not assessed
- Patients were enrolled only if diagnosed with FH or statin intolerance, two indications for which reimbursement for treatment is permitted.
- Altschmiedová T, Todorovová V, Šnejdrlová M, Šatný M, Češka R. PCSK9 inhibitors in real-world practice: Analysis of data from 314 patients and 2 years of experience in a center of preventive cardiology. Curr Atheroscler Rep. 2022 May;24(5):357–363. doi: 10.1007/s11883-022-01008-8. PMID: 35332442.

-from-the-SAFEHEART-registry.webp/jcr:content/Clinical%20practice%20experience%20in%20patients%20with%20familial%20hypercholesterolemia%20(FH)%20from%20the%20SAFEHEART%20registry.webp)