PCSK9i and Prevention of CVD
The synopsis of a Cochrane Systematic review on PCSK9 monoclonal antibodies for the primary and secondary prevention of cardiovascular disease.

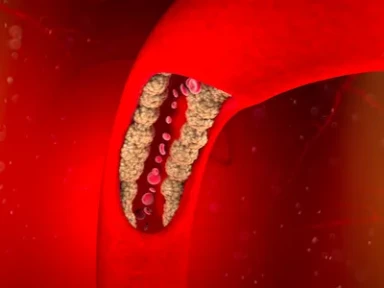
The study proved that the addition of PCSK9 inhibitors to traditional lipid-lowering therapies (LLTs) is set to reduce the risk of cardiovascular disease (CVD), including myocardial infarction (MI) and stroke, as well as all-cause mortality.
Key Takeaway
- This abridged version of a previously published Cochrane review highlighted the effect of adding PCSK9 inhibitors to traditional LLTs in reducing the risk of CVD, including MI and stroke, as well as all-cause mortality.
- High certainty evidence was noted for studies assessing the effect of PCSK9 inhibitors vs placebo when added to background statin or ezetimibe therapy.
- However, when PCSK9 inhibitors were directly compared with active treatment (either statins, ezetimibe or combination therapy), the evidence base was weaker and it was unclear if there was a protective or harmful effect in these patients.
- This review further noted the lack of sufficient data to exclude possible (long-term) safety signals on influenza, hypertension, cancer diagnosis or T2DM.
Why This Matters
- In patients with insufficient response to, or who are unable to tolerate traditional low-density lipoprotein-cholesterol (LDL-C)-lowering therapies (statins or ezetimibe), PCSK9 inhibitors may provide an alternative treatment.
- Present synopsis summarized the findings from a recent update of a Cochrane systematic review with focus on outcomes, safety, and the quality of evidence from the randomized clinical trials (RCTs) evaluating PCSK9 inhibitors.
Study Design
- Systematic review of 24 RCTs evaluating PCSK9 monoclonal antibodies for the primary and secondary prevention of CVDs:
- Databases: Cochrane Central Register of Controlled Trials, Medline, Embase, Web of Science, ClinicalTrials.gov and the International Clinical Trials Registry Platform
- Eligibility criteria: Parallel-group and factorial RCTs with at least 24 weeks of follow-up were eligible
- Exclusion criteria: Studies evaluating bococizumab and RG7652 (as these were discontinued)
- Primary outcomes: (1) Composite endpoint of CVD (defined as urgent coronary revascularization, unstable angina pectoris, non-fatal and fatal MI, non-fatal and fatal stroke, and coronary heart disease death); (2) all-cause mortality; (3) MI; and (4) stroke
- Secondary outcomes: (1) Influenza; (2) T2DM; (3) cancer; and (4) hypertension
Key Results
Predominantly high-risk patients were included in the RCTs evaluated in the Cochrane review (patients with non-optimal LDL-C concentration despite treatment with statins or ezetimibe, or with a history of CVD):
Patient characteristics
- Overall participants: N = 60,997 ([for whom this was reported: men = 71%; women = 29%; race/ethnicity = 83% Caucasian]; age = 61.57 vs 57.93 years)
- The study sample included:
- A total of 1,879 participants who had familial hypercholesterolemia (FH)
- 18,908 (31%) with a diagnosis of T2DM at baseline
- No prior history of CVD (n = 4,590)
Trial characteristics
- Alirocumab was evaluated in 18 trials, while evolocumab in 6 trials
- Comparator: Placebo in 18 trials, while ezetimibe and/or statins in 6 trials; study period: 2011–2018; setting: outpatient and home settings; countries: international
- PCSK9 inhibitors studied (randomization): Alirocumab = 43.5% participants; evolocumab = 56.5% participants
Key outcomes*
- PCSK9 inhibitors vs placebo (+background LLT [either statin, ezetimibe or a combination of these]): High certainty of evidence
- Composite endpoint of CVD (relative effect — odds ratio [OR {95% confidence interval; CI}]): Alirocumab vs placebo = 0.87 (0.80–0.94); evolocumab vs placebo = 0.84 (0.78–0.91)
- All-cause mortality (relative effect — OR [CI]): Alirocumab vs placebo = 0.83 (0.72–0.96); evolocumab vs placebo = 1.04 (0.91–1.19)
- MI (relative effect — OR [CI]): Alirocumab vs placebo = 0.86 (0.79–0.94); evolocumab vs placebo = 0.72 (0.64–0.82)
- Any stroke (relative effect — OR [CI]): Alirocumab vs placebo = 0.73 (0.58–0.91); evolocumab vs placebo = 0.79 (0.65–0.94)
Limitations
- Low/very low quality of evidence for studies directly comparing PCSK9 inhibitor efficacy with statins and/or ezetimibe (alirocumab: low; evolocumab: very low)
- Limited information was available regarding potential safety issues of either evolocumab or alirocumab
*Please refer the source publication (Carter et al.) for more details of the reported outcomes (including risk difference and certainty of evidence [Tables 1 and 2]).
- Carter JP, Hingorani AD, Wilkins J, Schmidt AF. Cochrane corner: PCSK9 monoclonal antibodies for the primary and secondary prevention of cardiovascular disease. Heart. 2022;108(1):14–15. doi: 10.1136/heartjnl-2021-319629. PMID: 34815331.

-from-the-SAFEHEART-registry.webp/jcr:content/Clinical%20practice%20experience%20in%20patients%20with%20familial%20hypercholesterolemia%20(FH)%20from%20the%20SAFEHEART%20registry.webp)