Global use of RAM and Thromboprophylaxis in hospitalized patients

Global use of risk assessment models and thromboprophylaxis in hospitalized patients with medical illnesses: An update from the World Thrombosis Day steering committee
This systematic review and meta-analysis revealed that anticoagulants are effective and safe for Venous Thromboembolism (VTE) prevention; however, thromboprophylaxis prescriptions are still unsatisfactory among hospitalized medically ill patients globally, with marked geographical differences.
Key Takeaway
-
This systematic review and meta-analysis of global studies indicates that:
-
In contrast to guideline recommendations, the frequency of thromboprophylaxis prescriptions was still unsatisfactory among hospitalized medically ill patients
-
Adequate thromboprophylaxis markedly varied across geographic regions
-
No major deviations were noted among risk assessment models
-
Most frequent reasons not to administer thromboprophylaxis: Active bleeding or a high risk of bleeding, including thrombocytopenia, and renal or liver dysfunction
-
The Padua Prediction score and the American College of Chest Physicians (ACCP) criteria were the most frequently adopted scores, followed by Caprini and Geneva scores
-
-
The World Thrombosis Day is instrumental for increasing VTE awareness and reducing disease burden.
Why This Matters
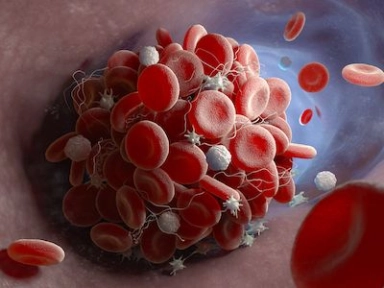
- VTE is a leading cause of cardiovascular morbidity and mortality.
-
In 2008, the Endorse study reported a substantial proportion of high-risk hospitalized patients, but a low use of appropriate thromboprophylaxis.
-
This systematic review and meta-analysis aimed at providing updated figures for the use of thromboprophylaxis and use of risk assessment models in acutely medically ill patients during hospitalization.
Study Design
- Search strategy: Trials, cohort studies, case-control studies, and surveys (not limited to English) from the past decade (2010) were searched in PubMed and Web of Science
- Inclusion criteria: (a) Observational non-randomized studies or surveys focusing on medically ill patients (e.g., those hospitalized for medical, non-surgical, condition); and (b) reporting the prevalent use of risk assessment models (with number of patients for each risk class) and of thromboprophylaxis
- Outcomes: (a) Patients with an indication for thromboprophylaxis based on individual risk assessment models or classifiers; (b) thromboprophylaxis use; and (c) reasons for not giving thromboprophylaxis to patients with another indication
Key Results
- In total, 27 studies from 20 countries (N = 137,288 patients) were included.
- Models used: Padua Prediction score (10 studies, n = 71,649); ACCP guideline-recommended scheme (10 studies, n = 4914); Caprini score (7 studies, n = 61,258); and Geneva score (1 study, n = 1478)
- Based on these models, 50.5% (95% confidence interval [CI]: 41.9–59.1, I2 = 99%) hospitalized medically ill patients were found to have high VTE risk.
-
Padua Prediction score: 30.4% (95% CI: 27.4–33.5, I2= 97%), Caprini score: 59.5% (95% CI: 34.9–81.8, I2 = 99%), ACCP criteria: 63.1% (95% CI: 52.3–73.4, I2= 98%)
-
-
Overall, 54.5% (95% CI: 46.2–62.6, I2 = 99%) of patients with high VTE risk received adequate thromboprophylaxis.
-
The frequency of thromboprophylaxis use was similar across groups: 56.9% (95% CI: 39.6–73.4, I2 = 99%) for Padua Prediction score, 53.8% (95% CI: 40.1–67.2, I2 = 98%) for ACCP criteria, and 50.5% (95% CI: 29.4–71.5, I2 = 99%) for Caprini score
-
Use of adequate thromboprophylaxis: Europe = 66.8% (95% CI: 50.7–81.1, I2 = 98%), Africa = 44.9% (95% CI: 31.8–58.4, I2 = 96%), Asia = 37.6% (95% CI: 25.7–50.3, I2 = 97%), South America = 58.3% (95% CI: 31.1–83.1, I2= 99%), North America = 68.6% (95% CI: 64.9–72.6, I2 = 96%)
-
-
Overall, 14 studies reported the frequency of relative and absolute contraindications to thromboprophylaxis.
-
Active bleeding was considered a contraindication in all studies.
-
Following active bleeding, the most prevalent contraindication was thrombocytopenia.
-
A bleeding disorder was reported as a contraindication in 7/11 studies.
-
In five studies, patients presenting with renal failure did not receive thromboprophylaxis.
-
Limitations
- Analysis only included observational studies.
- Some important studies were possibly not included.
- Risk assessment methods used for revaluating VTE risk were diverse.
- Cutoff for high-risk VTE and exclusion criteria was not homogeneously defined.
- High clinical and statistical heterogeneity were observed across studies.
- Forgo G, Micieli E, Ageno W, Castellucci LA, Cesarman-Maus G, Ddungu H, et al. An update on the global use of risk assessment models and thromboprophylaxis in hospitalized patients with medical illnesses from the World Thrombosis Day steering committee: Systematic review and meta-analysis. J Thromb Haemost. 2022;20(2):409–421. doi: 10.1111/jth.15607. PMID: 34822215.