Burdens of CSU

Patients with chronic spontaneous urticaria (CSU) endure a significant and multifaceted burden that worsens with disease severity1-4.
-
The condition impacts their Quality of Life (QoL) and health-related QoL (HRQoL) due to recurring, debilitating symptoms 1-4.
-
Additionally, CSU imposes a substantial financial and economic burden, further exacerbated by more severe cases5.

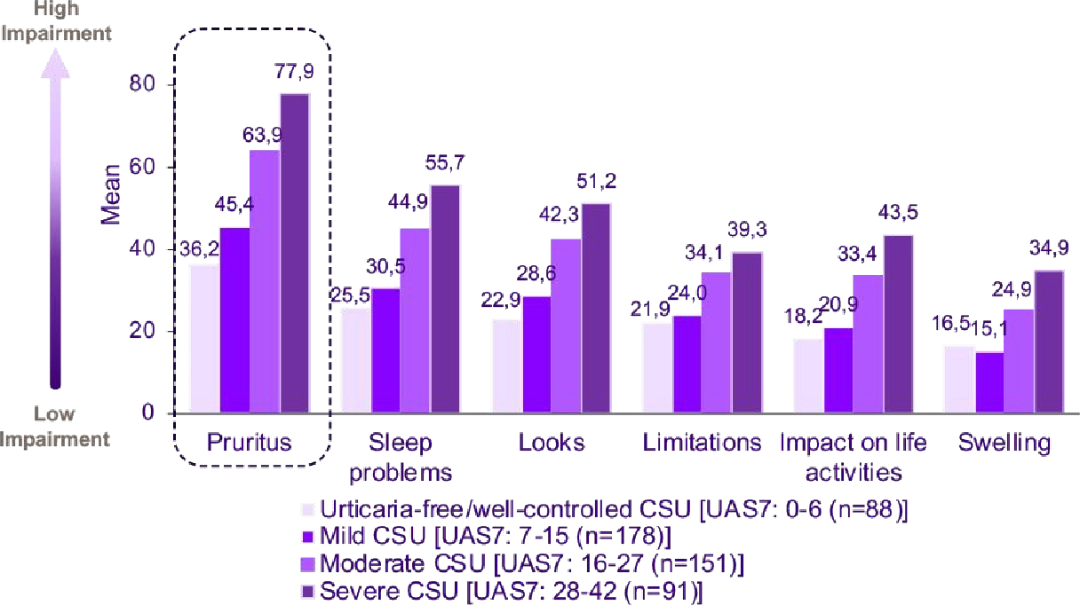
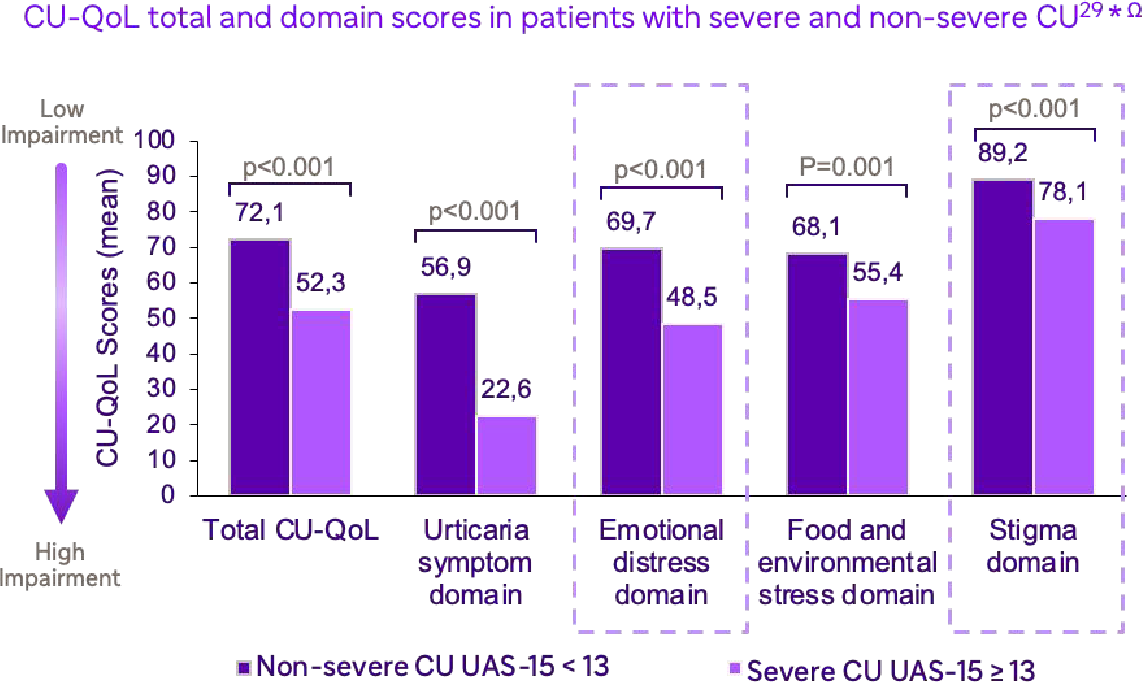
CU-Q2oL domain scores by disease severity42** ‡

Pruritic wheals:
- CSU is usually characterized by the presence of red, superficial, pruritic wheals and flare-type skin reactions12 that resolve and recur, migrating across the body12

Angioedema(Swelling of deep tissues):
- Angioedema may present alone11 or with wheals and is most frequently observed on the hands, face, and feet 13.
- Angioedema may be life-threatening if it affects the patient's airway14.
Spontaneous and transient development of wheals is a typical symptom of CSU, which is often concomitant with angioedema, and leads to a meaningful burden for patients 15,21.
 | Sudden, unpredictable, and transient outbreaks of wheals15 |
 | Visible lesions affecting numerous parts of the body (principally arms, legs, hands/ fingers and chest/abdomen)17 |
 | Daily recurrence for at least 6 weeks and often for many years16 |
 | Painful lesions associated with strong and persistent itching or burning sensation throughout the day15 |
Impact on Quality of Life
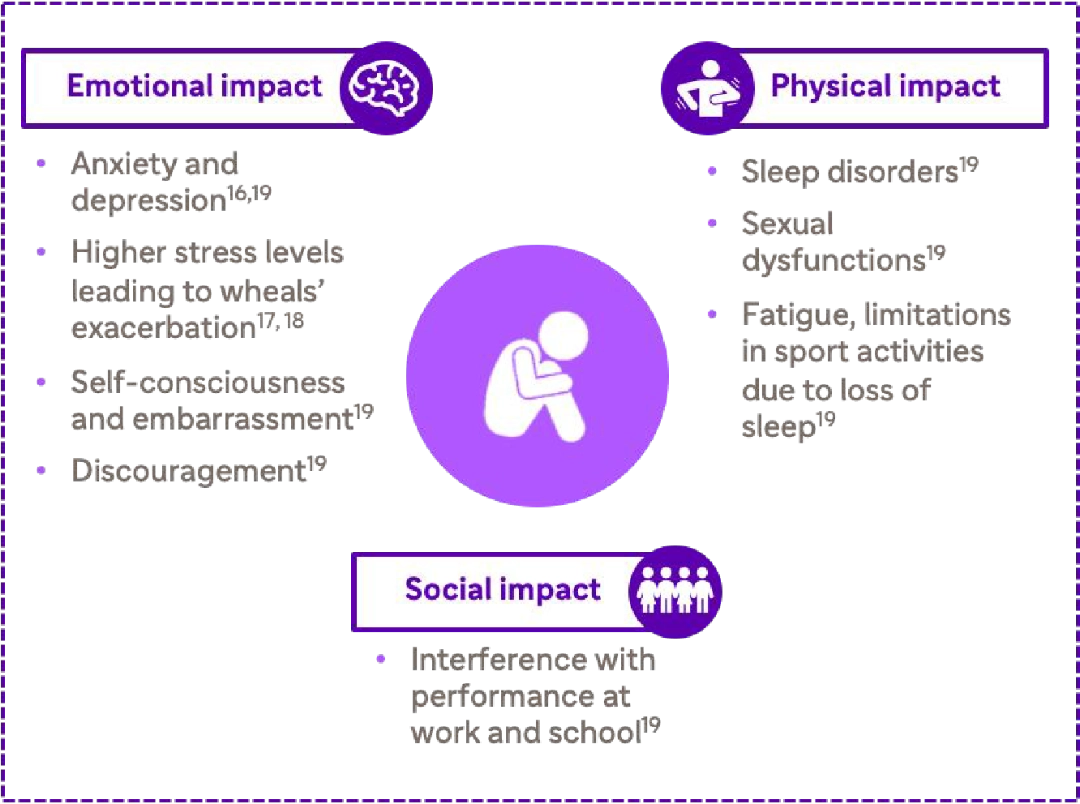
Chronic spontaneous urticaria (CSU) extends beyond its physical manifestations, profoundly impacting patients' emotional and psychological well-being22,23.
The persistent nature of CSU symptoms, including wheals and Angioedema, leads to significant distress that permeates various aspects of life.
Patients who experience concurrent wheals and angioedema represent approximately 40% of CSU patients and often face a longer duration of disease with a higher impact on QoL than patients who experience wheals only20,21.
CU-Q2oL domain scores by disease severity
Sleep disturbances are a key result of CSU symptoms, such as chronic pruritus, and increase with disease severity
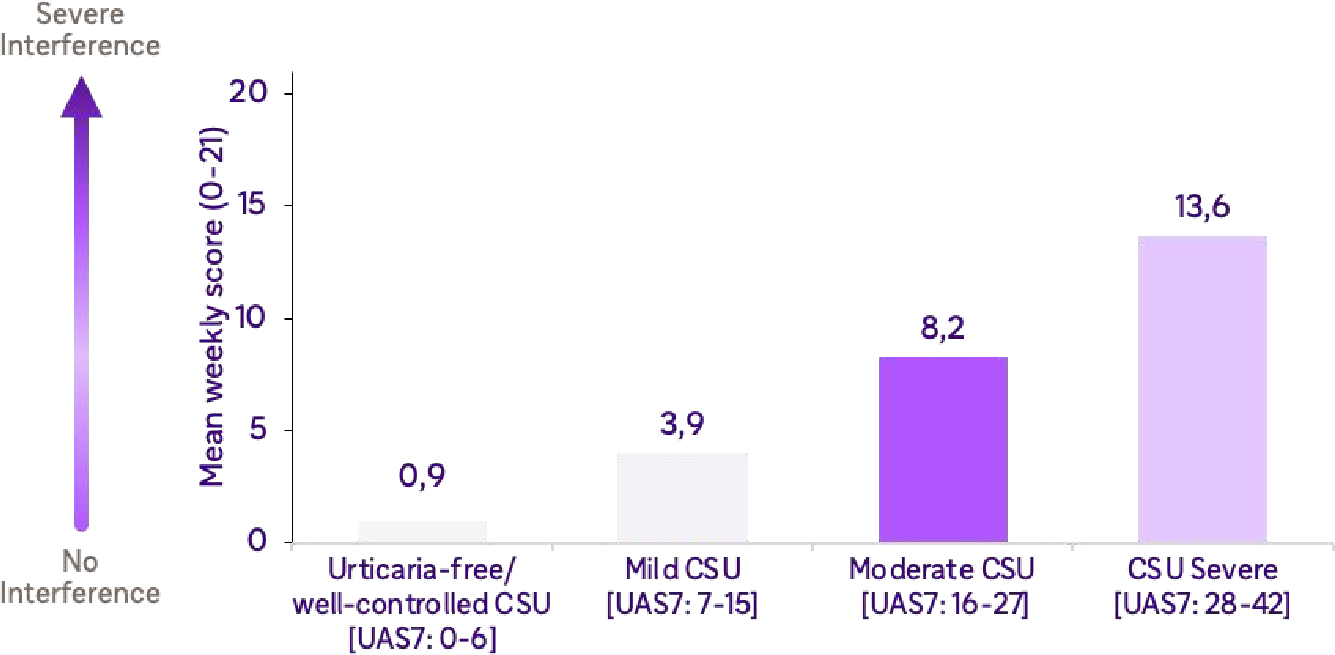
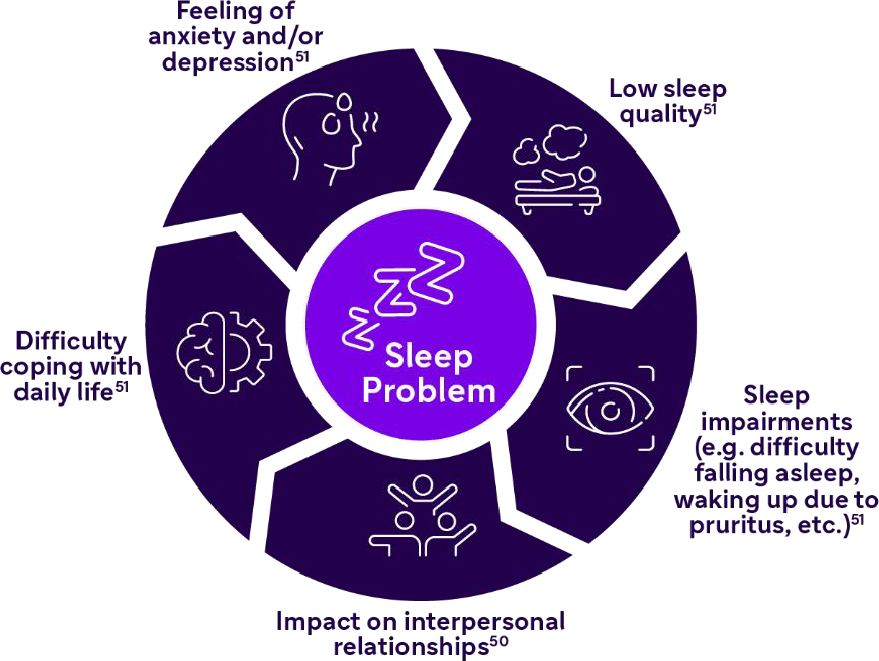
More than 50% of patients with CSU report sleep disturbances due to pruritus26,27, which often intensifies in the evenings and consequently affects other aspects of daily life, creating a vicious cycle of sleep problems25,28
Patients with CSU experience mental and emotional impairment, which increases with worsening disease severity and can disturb social interactions and lead to stigmatization 29,32.
Compared with the general population, patients with CSU have a higher prevalence of diagnosed psychiatric disorders30,33.

Distribution of psychiatric diagnosis among CSU patients30**
Note: **Data from a cross-sectional study (N=159) in Turkey from January 1 to April 20, 2005, which was collected via SF-36, and the SCID-I
Many patients with CSU feel that their unpredictable / uncontrollable symptoms exclude them from a normal lifestyle and are a source of frustration 31,32
 | 90% | of patients with CSU report that their symptoms place limitations on their normal physical activity, such as sports, hobbies, work, and sex31 |
 | 75% | of patients with CSU report having to miss out on social occasions because of their skin condition31 |
 | 56% | of patients with CSU report not having control over their symptoms31 |
 | 48% | of patients with CSU are unable to take part in usual social activities31 |
Financial Burden
The management of CSU imposes a financial burden on healthcare systems due to the increased number of physician visits, hospitalizations, and laboratory monitoring.
The economic burden is higher for patients with CSU than for individuals without CSU, due to increased healthcare visits and medication 34,35.
The mean all-cause healthcare cost for patients with CSU was found to be over $9,000 per patient per year35.
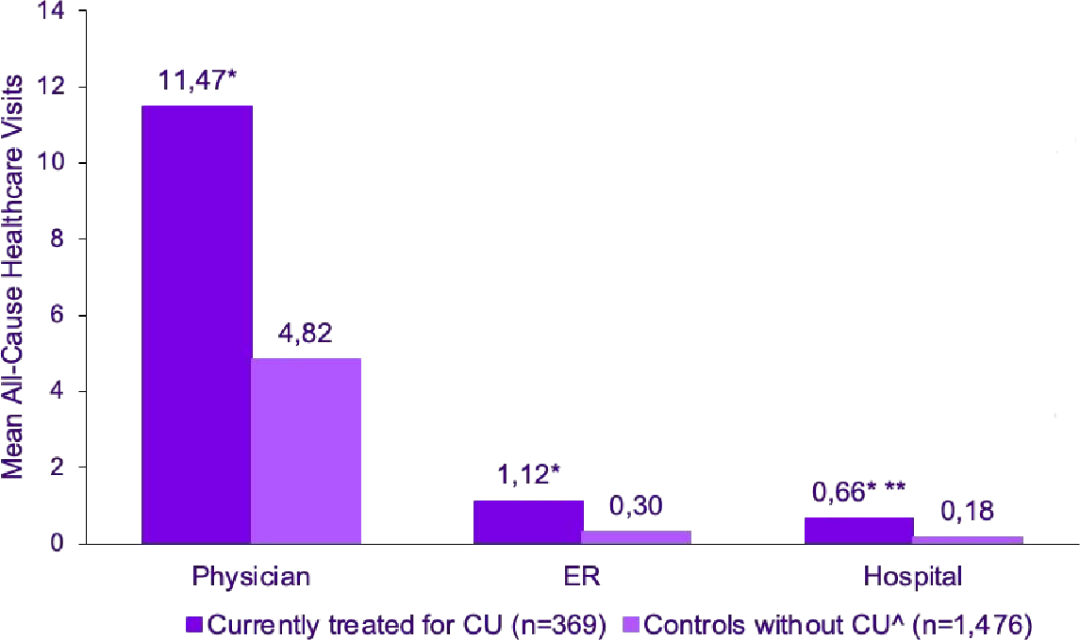
 | Number of all-cause healthcare visits during the prior 6 months34 ¥ |
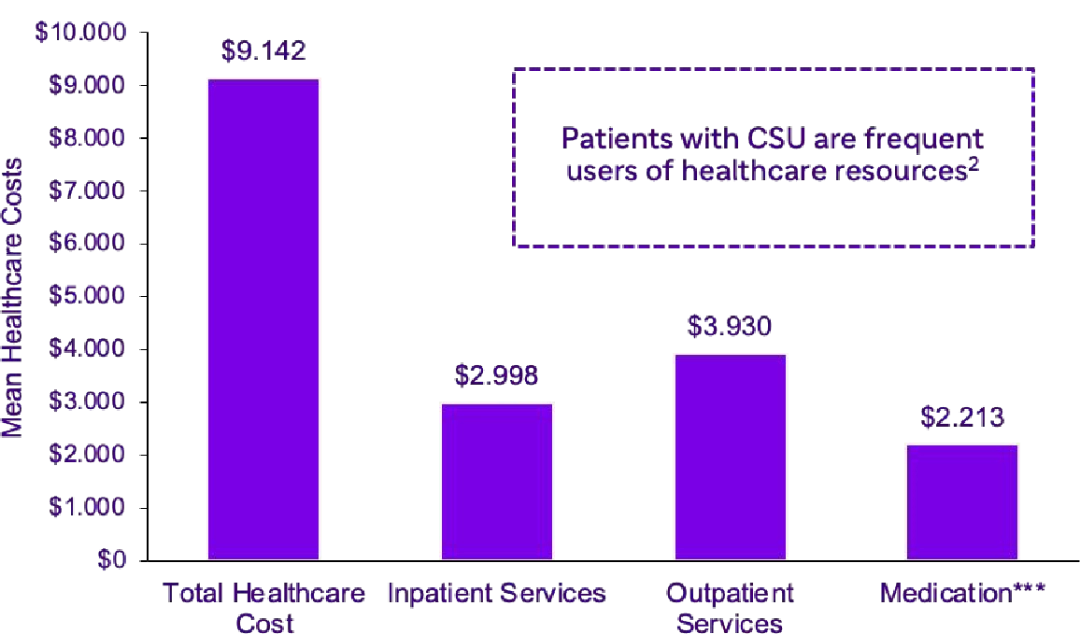
 | Mean annual healthcare costs by category in patients with CSU35 ‡ |
Notes: Data from the EU5 NHWS, which is a retrospective, cross-sectional study of patients who reported taking prescription medication for chronic hives identified as the proxy for patients with CSU (N=175,923) in the EU4 and in the UK in 2010, 2011 and 2013;
*Difference between the groups was significant, p-value<0.001; **p-value adjusted for violation of homogeneity of variance assumption;^Matched respondents to NHWS who had not experienced chronic urticaria; ‡p-values not provided, data is from a retrospective, cross-sectional cohort studv (N=6.350) in the US usina an existina database of commercial health insurance claims in 2012;***Accountina for Prescription medication onlv. as OTC medication (which includes most H1-AH) was not available in the database analyzed
Annual healthcare costs of CSU, including outpatient visits, laboratory monitoring costs, and out-of-pocket expenses, increase with worsening disease severity36,37.
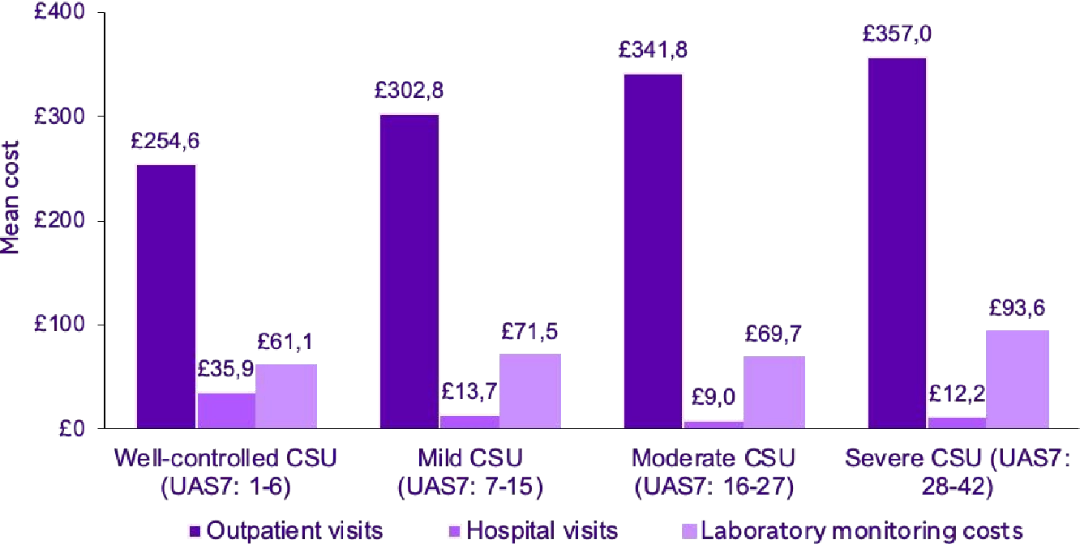
 | Annual direct healthcare costs by disease severity 36* |

As treatment many patients remain
symptomatic despite, many seek
alternative medical therapies which are
generally not covered by their country's
health insurances, resulting in additional
out-of-pocket expenses for patients,
estimated at $500-1,000/year37
Note: *Data from a Markov model consisting of health states based on UAS7 and additional states for relapse, spontaneous remission and death. Model cycle length was 4 weeks and the total model time horizon was 20 years in the base case. The model considered early discontinuation of non-responders (response: UAS7 ≤6) and retreatment upon relapse (relapse: UAS7 ≥16) for responders. Clinical and cost inputs were derived from omalizumab trials and published sources, and cost utility was expressed as ICERs. Scenario analyses included no early discontinuation of non-responders and an altered definition of response (UAS7 <16)
The management of CSU imposes a financial burden on healthcare systems due to the increased number of physician visits, hospitalizations, and laboratory monitoring38,39.

Note: *p-value<0.001; **p-value adjusted for violation of homogeneity of variance assumption; ¥Data from the EU4 and UK NHWS, which is a retrospective, cross-sectional study of patients (N=175,923) in the EU4 and UK in 2010, 2011 and 2013; Ω CU is used as a proxy for CSU; Matching variables used in matching were year of survey, country, age, and sex. Covariates included cigarette smoking, BMI category, and CCI score;‡p-value not provided in literature; Data from a retrospective medical record abstraction, a cross-sectional patient survey at enrolment and a patient diary completed over an 8-day period (twice daily assessment) after recruitment that included patients from the EU4, the UK, the Netherlands and Canada (N=673) from October 2013 to May 2015
- Maurer, M. Abuzakouk, F. Bérard, W. Canonica, H. Oude Elberink, A. Giménez-Arnau, C. Grattan, K. Hollis, A. Knulst, J.-P. Lacour, C. Lynde, A. Marsland, D. McBride, A. Nakonechna, J. Ortiz de Frutos, C. Proctor, G. Sussman, C. Sweeney, H. Tian, K. Weller, D. Wolin, M.-M. Bal. (2017). The burden of chronic spontaneous urticaria is substantial: Real-world evidence from ASSURE-CSU. Allergy, 72(12), 2005-2016. https://doi.org/10.1111/all.13209 [p2006/col1/h2, p2006/col2/h1, p2007/coll/h1, p2008/col1/h1, p2010/figure3B]
- Hawro, T., Przybytowicz, K., Spindler, M., Hawro, M., Stec, M., Altrichter, S., Weller, K., Magerl, M., Reidel, U., Alarbeed, E., Alraboni, O., Maurer, M., & Metz, M. (2021). The characteristics and impact of pruritus in adult dermatology patients: A prospective, cross-sectional study. Journal of the American Academy of Dermatology, 84(3), 691-700. https://doi.org/10.1016/j.jaad.2020.08.035 [p692/capsule summary/h1, p692/col2/h1]
- Allergy UK & Novartis. 2014. Wheals of Despair - Chronic Spontaneous Urticaria: breaking free from the cycle of despair. Available in : http:// preview.thenewsmarket.com/Previews/NVMC/DocumentAssets/333777.pdf [p6/col2/h3-4;p7/coll/h1-h3]
- Choi, W. S., Lim, E. S., Ban, G. Y., Kim, J. H., Shin, Y. S., Park, H. S., & Ye, Y. M. (2018). Disease-specific impairment of the quality of life in adult patients with chronic spontaneous urticaria. The Korean journal of internal medicine, 33(1), 185-192. https://doi.org/10.3904/kjim.2015.195 [p186/h1-h2; p189/h1]
- Broder, M. S., Raimundo, K., Antonova, E., & Chang, E. (2015). Resource use and costs in an insured population of patients with chronic idiopathic/ spontaneous urticaria. American journal of clinical dermatology, 16(4), 313-321. https://doi.org/10.1007/s40257-015-0134-8 [p313/abstract/h1, p314/col1/h1, p315/col2/h1, p316/col2/h1, p319/figure1]
- M. Maurer, M. Abuzakouk, F. Bérard, W. Canonica, H. Oude Elberink, A. Giménez-Arnau, C. Grattan, K. Hollis, A. Knulst, J.-P. Lacour, C. Lynde, A. Marsland, D. McBride, A. Nakonechna, J. Ortiz de Frutos, C. Proctor, G. Sussman, C. Sweeney, H. Tian, K. Weller, D. Wolin, M.-M. Balp. (2017). The burden of chronic spontaneous urticaria is substantial: Real-world evidence from ASSURE-CSU. Allergy, 72(12), 2005-2016. https://doi.org/10.1111/all.13209 [p2006/col1/h2, p2006col2/h1, p2007/col1/h1, p2007/col2/h1, p2010/fig3a]
- Hawro, T., Przybytowicz, K., Spindler, M., Hawro, M., Stec, M., Altrichter, S., Weller, K., Magerl, M., Reidel, U., Alarbeed, E., Alraboni, O., Maurer, M., & Metz, M. (2021). The characteristics and impact of pruritus in adult dermatology patients: A prospective, cross-sectional study. Journal of the American Academy of Dermatology, 84(3), 691-700. https://doi.org/10.1016/j.jaad.2020.08.035 [p691/abstract/h1-3; p692/capsule summary/h1; p692/coll/h1; p692/col3/h1; p697/ coll/h1-2; p697/col2/h1-2]
- Choi, W. S., Lim, E. S., Ban, G. Y., Kim, J. H., Shin, Y. S., Park, H. S., & Ye, Y. M. (2018). Disease-specific impairment of the quality of life in adult patients with chronic spontaneous urticaria. The Korean journal of internal medicine, 33(1), 185-192. https://doi.org/10.3904/kjim.2015.195 [p186/col1/h1]
- Saini S. S. (2014). Chronic spontaneous urticaria: etiology and pathogenesis. Immunology and allergy clinics of North America, 34(1), 33-52. https:// doi.org/10.1016/j.iac.2013.09.012 [p33/h2, p36/h1]
- Lavery, M. J., Kinney, M. O., Mochizuki, H., Craig, J., & Yosipovitch, G. (2016). Pruritus: an overview. What drives people to scratch an itch? The Ulster medical journal, 85(3), 164-173 [p164/col1/h1] ,
- Maurer, M., Weller, K., Bindslev-Jensen, C., et al. (2011). Unmet clinical needs in chronic spontaneous urticaria. A GA'LEN task force report. Allergy, 66(3), 317-330. https://doi.org/10.1111/j.1398-9995.2010.02496.x [p317/abstract/h1, p318/col1/h1]
- Yang, T. B., & Kim, B. S. (2019). Pruritus in allergy and immunology. The Journal of allergy and clinical immunology, 144(2), 353-360. https://doi.org/10.1016/ j.jaci.2019.06.016 [p3/h1]
- Hoskin, B., Ortiz, B., Paknis, B., & Kavati, A. (2019). Exploring the real-world profile of refractory and non-refractory chronic idiopathic urticaria in the USA: clinical burden and healthcare resource use. Current medical research and opinion, 35(8), 1387-1395. https://doi.org/10.1080/03007995.20191586222 [p1387/col1/h1]
- Radonjic-Hoesli, S., Hofmeier, K. S., Micaletto, S., Schmid-Grendelmeier, P., Bircher, A., & Simon, D. (2018). Urticaria and Angioedema: an Update on Classification and Pathogenesis. Clinical reviews in allergy & immunology, 54(1), 88-101. https://doi.org/10.1007/s12016-017-8628-1 [p3/col1/h1-2]
- Radonjic-Hoesli, S., Hofmeier, K. S., Micaletto, S., Schmid-Grendelmeier, P., Bircher, A., & Simon, D. (2018). Urticaria and Angioedema: an Update on Classification and Pathogenesis. Clinical reviews in allergy & immunology, 54(1), 88-101. https://doi.org/10.1007/s12016-017-8628-1 [p89/col1/h1]
- Allergy UK & Novartis. 2014. Wheals of Despair - Chronic Spontaneous Urticaria: breaking free from the cycle of despair. Available in : http:// preview.thenewsmarket.com/Previews/NVMC/DocumentAssets/333777.pdf [p2/col1/h1, p6/col1/h1, p7/col1/h1-2]
- Wagner, N. (2021). Patients with Chronic Urticaria Remain Largely Undertreated: Results from the DERMLINE Online Survey. (2021). Springermedizin.de. https://www.springermedizin.de/patients-with-chronic-urticaria-remain-largely-undertreated-resu/19131558 [p1035/col2/h1]
- Conrad, R. (2008). Relationship between anger and pruritus perception in patients with chronic idiopathic urticaria and psoriasis. Academia. https:// www.academia.edu/30625027/Relationship_between_anger_and_pruritus_perception_in_patients_with_chronic_idiopathic_urticaria_and_psoriasis [p1065/col2/h1]
- Gonçalo, M., Gimenéz-Arnau, A., Al-Ahmad, M., Ben-Shoshan, M., Bernstein, J., Ensina, L., Fomina, D., Galvàn, C., Godse, K., Grattan, C., Hide, M., Katelaris, C., Khoshkhui, M., Kocatürk, E., Kulthanan, K., Medina, I., Nasr, I., Peter, J., Staubach, P., Wang, L., Weller, K. and Maurer, M. (2020). The global burden of chronic urticaria for the patient and society*. British Journal of Dermatology, 184(2), 226-236. https://doi.org/10.1111/bjd.19561 [p230/col1/h1-3, p231/col1/h1, p231/col2/h1]
- Sussman, G., Abuzakouk, M., Bérard, F., Canonica, W., Oude Elberink, H., Giménez-Arnau, A., Grattan, C., Hollis, K., Hunter, S., Knulst, A., Lacour, J. P., Lynde, C., Marsland, A., McBride, D., Maurer, M., Nakonechna, A., Ortiz de Frutos, J., Reynolds, M., Sweeney, C., Tian, H.,... Balp, M. M. (2018). Angioedema in chronic spontaneous urticaria is underdiagnosed and has a substantial impact: Analyses from ASSURE-CSU. Allergy, 73(8), 1724-1734. https://doi.org/10.1111/ all.13430 [p1725/coll/h1, p1725/col2/h1]
- Powell, R. J., Leech, S. C., Till, S., Huber, P. A., Nasser, S. M., Clark, A. T. (2015). BSACI guideline for the management of chronic urticaria and angioedema. Clinical and experimental allergy: journal of the British Society for Allergy and Clinical Immunology, 45(3), 547-565. https://doi.org/10.1111/cea.12494 [p549/ coll/h1]
- Tzur Bitan, D., Berzin, D., & Cohen, A. (2020). The association of chronic spontaneous urticaria (CSU) with anxiety and depression: A nationwide cohort study. Archives of Dermatological Research, 312(5), 339-344. https://doi.org/10.1007/s00403-020-02064-3
- Dias, G. A. C., Pires, G. V., Rodrigues do Valle, S. O., Dortas Júnior, S. D., Levy, S., França, A. T., Baiardini, I., & Canonica, W. G. (2016). Impact of chronic urticaria on the quality of life of patients followed up at a university hospital. Annals of Dermatology, 28(6), 733-739. https://doi.org/10.5021/ ad.2016.28.6.733
- M. Maurer, M. Abuzakouk, F. Bérard, W. Canonica, H. Oude Elberink, A. Giménez-Arnau, C. Grattan, K. Hollis, A. Knulst, J.-P. Lacour, C. Lynde, A. Marsland, D. McBride, A. Nakonechna, J. Ortiz de Frutos, C. Proctor, G. Sussman, C. Sweeney, H. Tian, K. Weller, D. Wolin, M.-M. Balp. (2017). The burden of chronic spontaneous urticaria is substantial: Real-world evidence from ASSURE-CSU. Allergy, 72(12), 2005-2016. https://doi.org/10.1111/all.13209 [p2006/col1/h2; p2006/col2/h1, p2007/coll/h1, p2007/col2/h1, p2011/figure3D]
- Zuberbier, T., Abdul Latiff, A. H., Abuzakouk, M., et al. (2022). The international EAACI/GA'LEN/EuroGuiDerm/APAAACI guideline for the definition, classification, diagnosis, and management of urticaria. Allergy, 77(3), 734-766. https://doi.org/10.1111/all.15090 [p14/col2/h1, p18/table10]
- He, G. Y., Tsai, T. F., Lin, C. L., Shih, H. M., & Hsu, T. Y. (2018). Association between sleep disorders and subsequent chronic spontaneous urticaria development: A population-based cohort study. Medicine, 97(34), e11992. https://doi.org/10.1097/MD.0000000000011992.[p1/col2/h1]
- Gonçalo, M., Gimenéz-Arnau, A., Al-Ahmad, M., Ben-Shoshan, M., Bernstein, J. A., Ensina, L. F., Fomina, D., Galvàn, C. A., Godse, K., Grattan, C., Hide, M., Katelaris, C. H., Khoshkhui, M., Kocatürk, E., Kulthanan, K., Medina, I., Nasr, I., Peter, J., Staubach, P., Wang, L., ... Maurer, M. (2021). The global burden of chronic urticaria for the patient and society. The British journal of dermatology, 184(2), 226-236. [p230/coll/h3, p231/col1/h1]
- Hawro, T., Przybytowicz, K., Spindler, M., Hawro, M., Stec, M., Altrichter, S., Weller, K., Magerl, M., Reidel, U., Alarbeed, E., Alraboni, O., Maurer, M., & Metz, M. (2021). The characteristics and impact of pruritus in adult dermatology patients: A prospective, cross-sectional study. Journal of the American Academy of Dermatology, 84(3), 691-700. https://doi.org/10.1016/j.jaad.2020.08.035 [p691/abstract/h2-3, p697/col2/h1-2]
- Choi WS, Lim ES, Ban GY, Kim JH, Shin YS, Park HS, Ye YM. Disease-specific impairment of the quality of life in adult patients with chronic spontaneous urticaria. Korean J Intern Med. 2018 Jan;33(1):185-192 [р185/abstract/h1, p186/coll/h2, p188/figure2]
- Ozkan, M., Oflaz, S. B., Kocaman, N., Ozseker, F., Gelincik, A., Büyüköztürk, S., Ozkan, S., & Colakoglu, B. (2007). Psychiatric morbidity and quality of life in patients with chronic idiopathic urticaria. Annals of allergy, asthma & immunology: official publication of the American College of Allergy, Asthma, & Immunology, 99(1), 29-33. https://doi.org/10.1016/S1081-1206(10)60617-5 [p29/abstract/h1, p31/table2]
- Allergy UK & Novartis. 2014. Wheals of Despair - Chronic Spontaneous Urticaria: breaking free from the cycle of despair. Available in : http:// preview.thenewsmarket.com/Previews/NVMC/DocumentAssets/333777.pdf [p7/col1/h1-3; p8/h1-3]
- Gonçalo, M., Gimenéz-Arnau, A., Al-Ahmad, M., Ben-Shoshan, M., Bernstein, J. A., Ensina, L. F., Fomina, D., Galvàn, C. A., Godse, K., Grattan, C., Hide, M., Katelaris, C. H., Khoshkhui, M., Kocatürk, E., Kulthanan, K., Medina, I., Nasr, I., Peter, J., Staubach, P., Wang, L., ... Maurer, M. (2021). The global burden of chronic urticaria for the patient and society. The British journal of dermatology, 184(2), 226-236. [p230/col1/h1-2, p231/col1/h1]
- Sansone, R. A., & Sansone, L. A. (2010). Psychiatric disorders: a global look at facts and figures. Psychiatry (Edgmont (Pa. : Township)), 7(12), 16-19 [p17/col1/ h1]
- Balp, M. M., Vietri, J., Tian, H., & Isherwood, G. (2015). The Impact of Chronic Urticaria from the Patient's Perspective: A Survey in Five European Countries. The patient, 8(6), 551-558. https://doi.org/10.1007/s40271-015-0145-9 [p551/abstract/h1-2, p552/col2/h1-3, p554/coll/h1, p557/table5]
- Broder, M. S., Raimundo, K., Antonova, E., & Chang, E. (2015). Resource use and costs in an insured population of patients with chronic idiopathic/ spontaneous urticaria. American journal of clinical dermatology, 16(4), 313-321. https://doi.org/10.1007/s40257-015-0134-8 [p313/abstract/h1, p314/col1/h1, p315/col2/h1, p316/col2/h1, p319/figure1]
- Graham, J., McBride, D., Stull, D., Halliday, A., Alexopoulos, S. T., Balp, M. M., Griffiths, M., Agirrezabal, I., Zuberbier, T., & Brennan, A. (2016). Cost Utility of Omalizumab Compared with Standard of Care for the Treatment of Chronic Spontaneous Urticaria. PharmacoEconomics, 34(8), 815-827. https:// doi.org/10.1007/s40273-016-0412-1 [p815/abstract/h1; p821/table3]
- M. Maurer, M. Abuzakouk, F. Bérard, W. Canonica, H. Oude Elberink, A. Giménez-Arnau, C. Grattan, K. Hollis, A. Knulst, J.-P. Lacour, C. Lynde, A. Marsland, D. McBride, A. Nakonechna, J. Ortiz de Frutos, C. Proctor, G. Sussman, C. Sweeney, H. Tian, K. Weller, D. Wolin, M.-M. Balp. (2017). The burden of chronic spontaneous urticaria is substantial: Real-world evidence from ASSURE-CSU. Allergy, 72(12), 2005-2016. https://doi.org/10.1111/all.13209 [p2006/col1/h2, p2006/col2/h1, p2007/col1/h1, p2013/col1/h1]
- Balp, M. M., Vietri, J., Tian, H., & Isherwood, G. (2015). The Impact of Chronic Urticaria from the Patient's Perspective: A Survey in Five European Countries. The patient, 8(6), 551-558. https://doi.org/10.1007/s40271-015-0145-9 [p552/col2/h1-3; p554/coll/h1; p556/table4]
- M. Maurer, M. Abuzakouk, F. Bérard, W. Canonica, H. Oude Elberink, A. Giménez-Arnau, C. Grattan, K. Hollis, A. Knulst, J.-P. Lacour, C. Lynde, A. Marsland, D. McBride, A. Nakonechna, J. Ortiz de Frutos, C. Proctor, G. Sussman, C. Sweeney, H. Tian, K. Weller, D. Wolin, M.-M. Balp. (2017). The burden of chronic spontaneous urticaria is substantial: Real-world evidence from ASSURE-CSU. Allergy, 72(12), 2005-2016. https://doi.org/10.1111//all.13209 [p2006/col1/h2, p2006/col2/h1, p2007/coll/h1, p2008/col2/h1]