- Article
- Source: Campus Sanofi
- 23 Oct 2023
Signs and Symptoms of Pompe disease

Pompe disease should be considered as part of the differential diagnosis for all children and adults presenting with limb-girdle muscle weakness and respiratory insufficiency1
Watch the below video to find out more about when to suspect Pompe disease
Late Onset Pompe Disease (LOPD)
The most common clinical manifestations are progressive proximal muscle weakness and respiratory insufficiency2
Respiratory muscle weakness
In a study of 92 children and adults with untreated LOPD, 74% of all patients had pulmonary dysfunction3

Proximal muscle weakness
In a study of 94 adults with LOPD, shoulder, abdominal, paraspinal, and hip muscles were weakened in >80% of patients4
Respiratory muscle weakness
In a study of 92 children and adults with untreated LOPD, 74% of all patients had pulmonary dysfunction3

Proximal muscle weakness
In a study of 94 adults with LOPD, shoulder, abdominal, paraspinal, and hip muscles were weakened in >80% of patients4

Testing and Diagnosis of Pompe disease

Testing and Diagnosis of Pompe disease
Progressive proximal muscle weakness and respiratory insufficiency2 ultimately lead to a loss of ambulation and the need for ventilation support. Children and adults with Pompe disease show much greater heterogeneity than infants with the condition.2,5,4
In practice, some of the visible signs and symptoms you may see in people with Pompe, include a waddling gait and difficulty rising from a standing position. Watch the following videos to see how these symptoms may present:
Gower's maneuver (reliance on the upper body to rise from a seated position)
Myopathic gait (imbalances walking due to weakness in the limb-girdle)
As the disease progress' difficulty climbing stairs will become more pronounced
As will difficulty reaching overhead
Some of the symptoms people with late-onset Pompe disease may experience include2
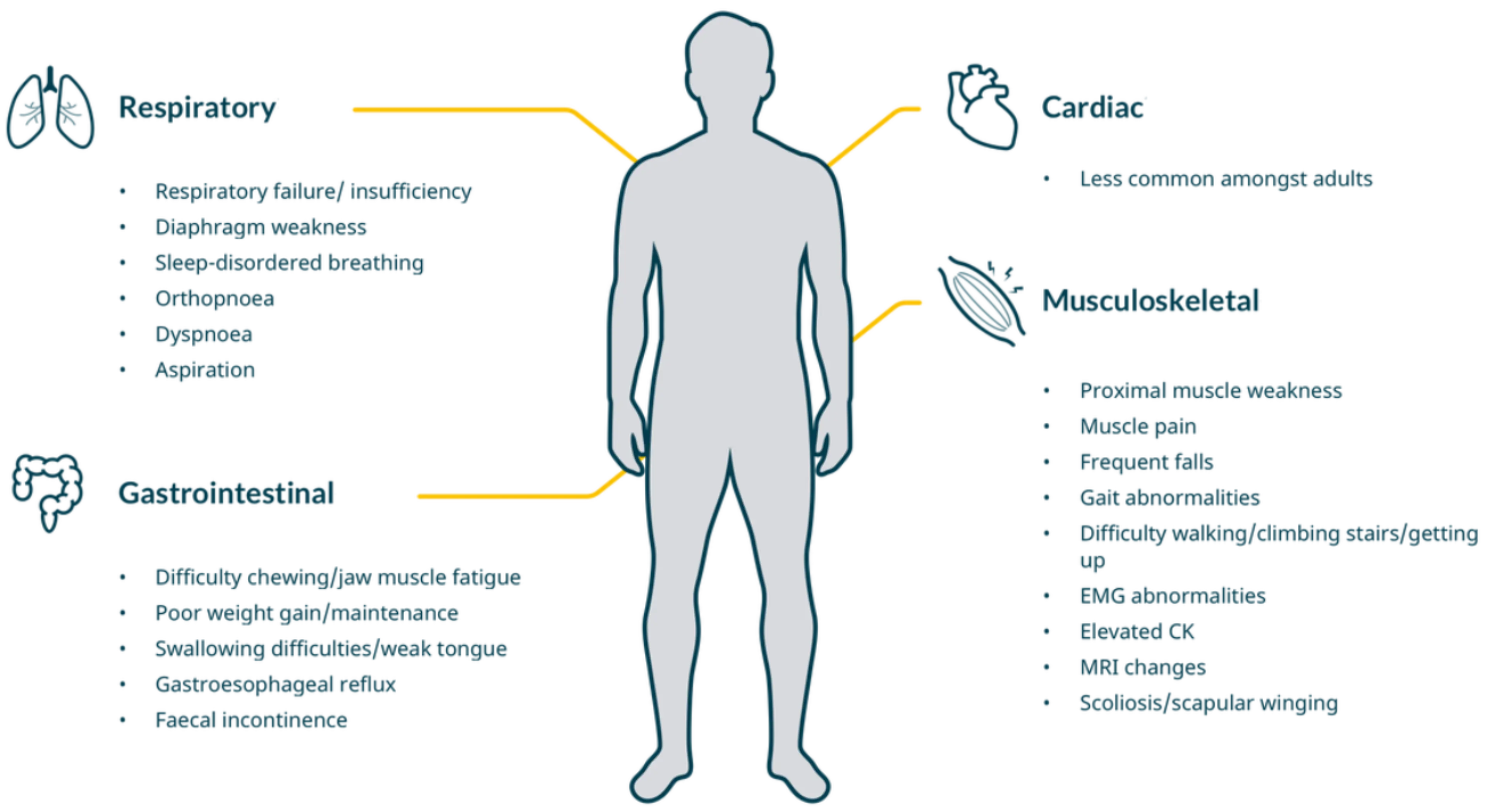
Cardiac involvement is rare in children and in adults with Late-Onset Pompe disease but pronounced in infantile onset.
Infantile Onset Pompe Disease (IOPD) – infants typically present with pronounced hypotonia, severe cardiomegaly8 and cardiomyopathy6
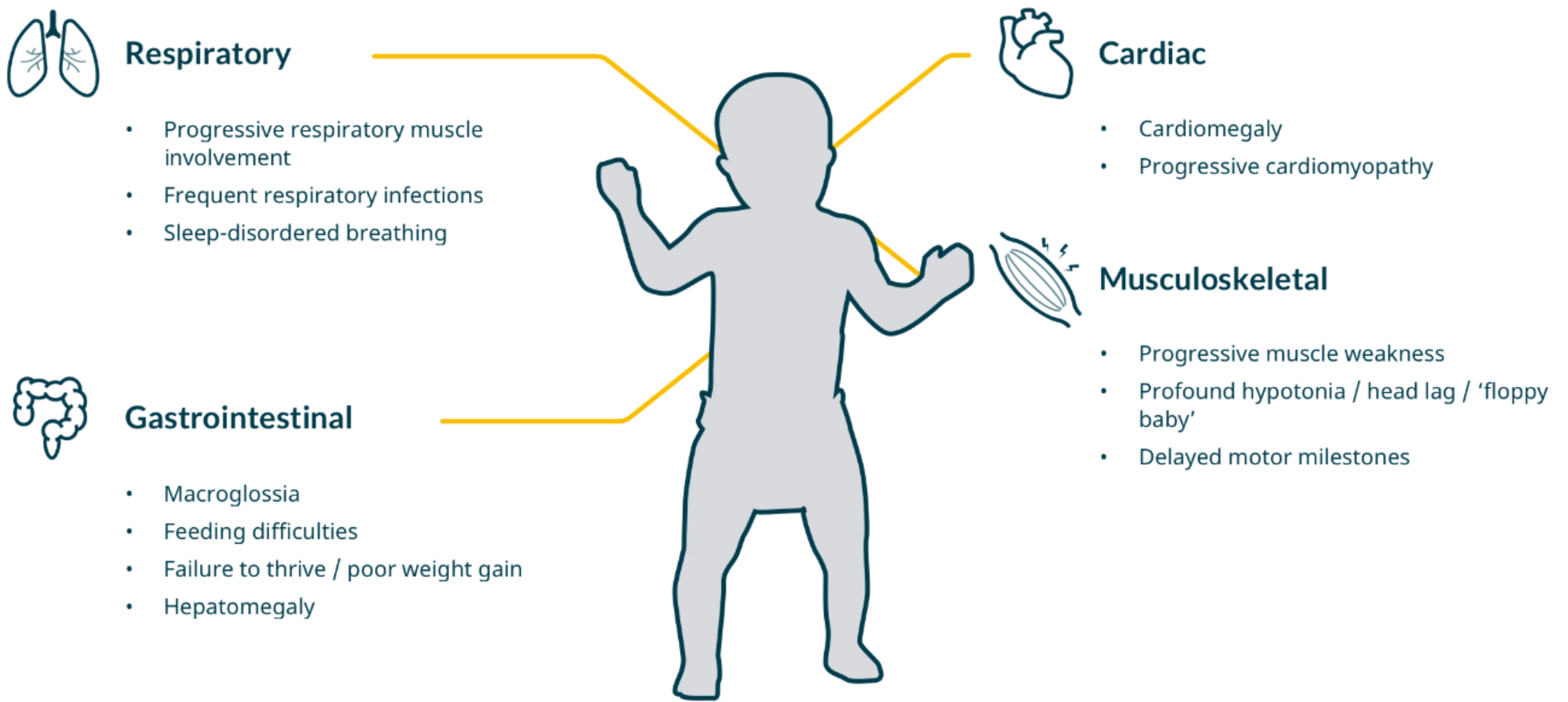
- Other signs include frequent respiratory infections, failure to reach motor milestones and difficulty feeding
- Patients with Pompe disease will exhibit progressive muscular weakness
- Pompe disease most commonly affects the proximal limbs and respiratory muscles, no matter the age of the patient6

Testing and Diagnosis of Pompe disease

Testing and Diagnosis of Pompe disease
Respiratory
Respiratory manifestations caused by diaphragm weakness can be the first indication of Pompe disease9-11
If left untreated, Pompe disease can lead to respiratory failure – the most common cause of death in Pompe disease2,10-12 |
Patients may notice the first signs of respiratory muscle dysfunction when lying down, including:10,12,13
Orthopnoea
Hypoventilation, especially when lying down

Sleep disordered breathing (SDB)

Morning headache

Dyspnoea at rest and after exercise

Chronic respiratory insufficiency
Orthopnoea
Hypoventilation, especially when lying down

Sleep disordered breathing (SDB)

Morning headache

Dyspnoea at rest and after exercise

Chronic respiratory insufficiency
Look out for other symptoms which may point towards Pompe disease:
- Reduced postural drop in forced vital capacity (FVC) of 25% from the sitting to the supine position4,14,15
- Susceptibility to chest infections11
- Post-operative failure to wean on to solid food due to muscle weakness16

Difficulty weaning a patient off ventilators16

Difficulty weaning a patient off ventilators16
References
- American Association of Neuromuscular & Electrodiagnostic Medicine. Muscle Nerve 2009; 40(1):149–160
- Winkel LP, et al. J Neurol. 2005;252 (8):875–884
- van der Beek NA, et al. Mol Genet Metab. 2011;104(1-2):129–136
- van der Beek NA, et al. Orphanet J Rare Dis. 2012 ;7:88
- American Association of Neuromuscular & Electrodiagnostic Medicine. Muscle Nerve 2009; 40(1):149–160
- Hirschhorn R, et al. The Metabolic and Molecular Basis of Inherited Disease 2001;8(3):3389–3420
- Kishnani PS, et al. Genet Med. 2006; 8(5):267–288
- Kishnani PS, et al. J Pediatr. 2006; 148:671–676
- Muller-Felber W, et al. Neuromuscul Disord. 2007;17(9-10):698–706
- Fuller D, et al. Respir Physiol Neurobiol. 2013;189(2):241–249
- Mellies U, et al. Respir Med. 2009;103(4):477–484
- Sixel B de S, et al. Jornal Brasileiro de Pneumologia 2017;43(1):54–59
- O’Callaghan C, et al. Respirology Case Reports 2016;4(5):e00178
- Manganelli F, et al. Acta Myol. 2013;32(2):82–84
- Gaeta M, et al. Mol Genet Metab. 2013;110(3):290–296
- Ruiz A, et al. PM&R. 2014;6(8 Suppl. 2):S 100
MAT-XU-2202603 (v2.0) Date of preparation: October 2023