- Article
- Source: Campus Sanofi
- 23 Oct 2023
Testing and Diagnosis of Pompe disease

Testing
Start with a simple, reliable blood-based test
GAA assays using whole blood or dried blood spot (DBS) samples are an established diagnostic method for Pompe disease.1,2
Muscle biopsy is less reliable than a blood-based test for Pompe disease because it can miss more than one third (37%) of positive diagnoses.2-4

Acid alpha-glucosidase activity assay is the gold standard for Pompe disease diagnosis.5
Why not rule out Pompe disease early by incorporating a blood-based assay in your differential diagnosis? |

Other tests to consider include:
- Biopsies (skin and muscle), although these can be invasive for the patient and potentially inconclusive6,7
- Genetic testing
- Next Generation Sequencing (NGS), which can be used to quickly analyse a person’s genome to determine a diagnosis8

Why test early for Pompe disease?

Why test early for Pompe disease?
Diagnosis
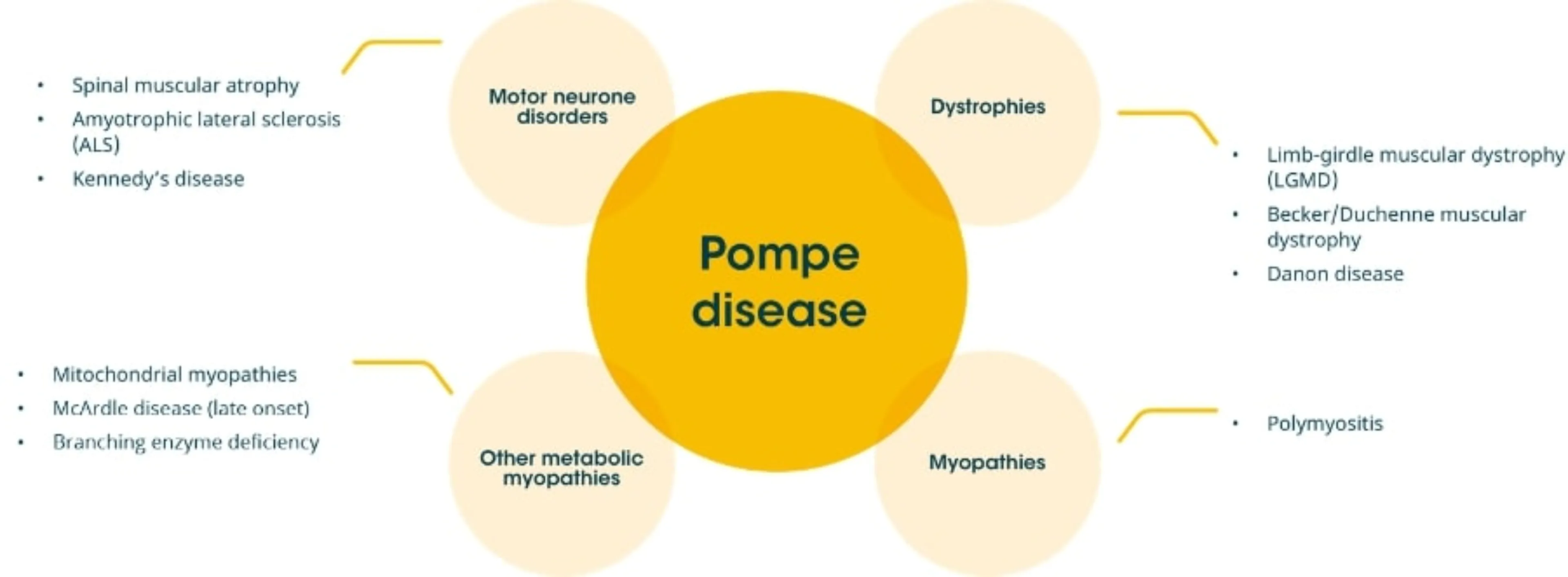
Diagnosing Pompe disease can be challenging due to:

Overlap of symptoms with other neuromuscular disorders3
Heterogeneity of presentation (broad spectrum of clinical phenotypes)9-10

Overlap of symptoms with other neuromuscular disorders3
Heterogeneity of presentation (broad spectrum of clinical phenotypes)9-10
Unlike other neuromuscular disorders, respiratory symptoms are often one of the first clinical manifestations of Pompe disease, and may precede proximal muscle weakness11,12
Pompe disease shares similar signs and symptoms with a number of the other conditions and should be considered as part of the differential diagnosis for all children and adults presenting with limb-girdle weakness and/or respiratory insufficiency.3
|
Patient Presentation/Symptoms |
# of patients |
% with Pompe Disease |
|
Undefined limb-girdle myopathy or undiagnosed proximal muscle weakness (2013)13 |
144 |
10.2% |
|
Unclassified limb-girdle muscular dystrophy (2013)14 |
38 |
8.0% |
|
Idiopathic hyperCKemia or newly presenting patients with hyperCKemia (2013)13 |
207 |
2.4% |
|
Asymptomatic hyperCKemia of unknown cause (2013)16 |
137 |
1(0.9)% |
|
HyperCKemia and no clinical muscle weakness (2006)17 |
104 |
3.8% |
Patients with Pompe disease often face delayed diagnosis, it should be considered when signs and symptoms suggest progressive muscular degeneration in infants, children, adolescents and adults18,19
The ability to correctly differentiate Pompe disease from other disorders is crucial for minimising diagnostic delays and optimising patient outcomes and the earlier a patient receives treatment, the better their long-term prognosis.
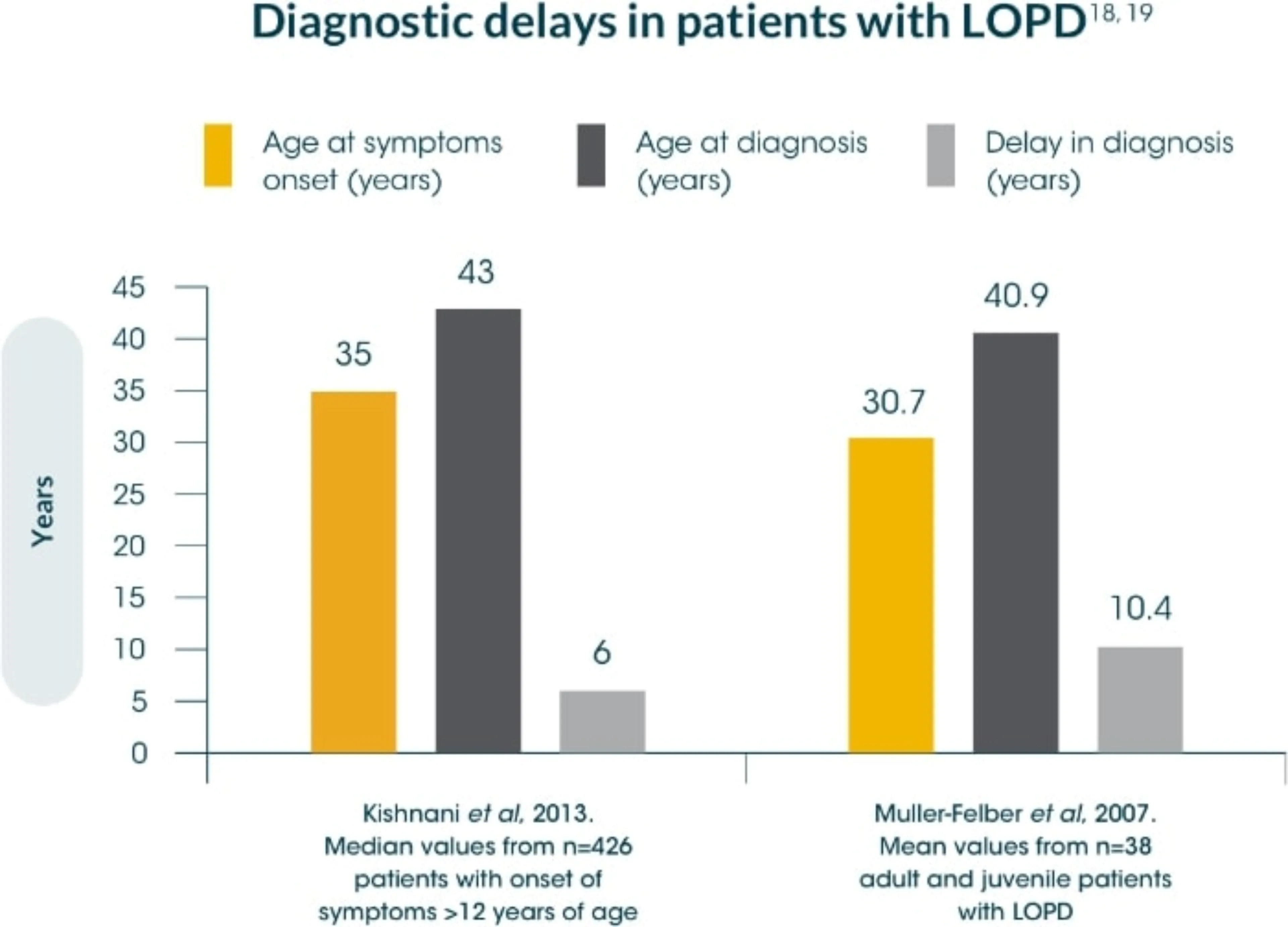
Delayed diagnosis can lead to significant muscle tissue deterioration21, diminished physical function, and premature death3,18,19,20
Due to the overlapping symptoms of Pompe disease and other neuromuscular conditions, consider re-examining some patients to rule out Pompe disease, including those with:
- Unspecified limb-girdle myopathies13-15
- Unexplained respiratory problems22
- Unexplained skeletal muscle problems22
- Patients with hyperCKemia13,16,17

In a prospective cohort screening study of 3,076 patients tested with dried blood spot, 74 patients were diagnosed with Pompe disease. From this study, 2.4% of patients with unclassified limb-girdle muscle weakness was found to be Pomep disease. It was therefore concluded that when patients present with limb-girdle muscle weakness routine testing for Pompe disease should occur.23

In a prospective cohort screening study of 3,076 patients tested with dried blood spot, 74 patients were diagnosed with Pompe disease. From this study, 2.4% of patients with unclassified limb-girdle muscle weakness was found to be Pomep disease. It was therefore concluded that when patients present with limb-girdle muscle weakness routine testing for Pompe disease should occur.23
References
-
Hobson-Webb LD, et al. Muscle Nerve 2012;45(2):301–302
-
Vissing J, et al. JAMA Neurol. 2013;70(7):923–927
-
American Association of Neuromuscular & Electrodiagnostic Medicine. Muscle Nerve 2009;40(1):149–160
-
Laforêt P, et al. Rev Neurol. (Paris) 2013;169(8-9):595–602
-
Manganelli F and Ruggiero L. Acta Myol. 2013;32(2):82–84.
-
Zhang H, et al. Genet Med. 2006;8:302–306
-
Winchester B, et al. Mol Genet Metab. 2008;93(3):275–281
-
Behjati S, et al. Arch Dis Child Educ Pract Ed. 2013;98(6):236–238
-
Hirschhorn R, et al. The Metabolic and Molecular Basis of Inherited Disease 2001;8(3):3389–3420
-
Hagemans ML, et al. Neurology 2006;66(4):581-583
-
Mellies U, et al. Respir Med. 2009;103(4):477–484
-
Culper EJ, et al. Muscle Nerve 2012;45(3):319-333
-
Bautista Lorite J. Expert Rev Neur Ed Especial. 2013;13:17–19
-
Preisler N, et al. Mol Genet Metab. 2013;110(3):287-9
-
Goldstein JL, et al. Muscle Nerve 2009;40(1):32–36
-
Spada M, et al. Mol Genet Metab. 2013;109(2):171–173
-
Fernandez C, et al. Neurology. 2006;66(10):1585–1587
-
Winkel LP, et al. J Neurol. 2005;252(8):875–884
-
Kishnani PS, et al. Genet Med. 2006;8(5):267–288
-
Kishnani PS, et al. Am J Med Genet A. 2013;161A(10):2431–2443
-
Muller-Felber W, et al. Neuromuscul Disord. 2007;17:698–706
-
Toscano A, et al. J Neurol. 2013;260(4):951–959
-
Lukacs et al. 2016. Neurology; 87(3):295-298
MAT-XU-2202605 (v2.0) Date of preparation: October 2023