Use of Ticagrelor vs clopidogrel use in high bleeding risk in hospitalized patients with acute coronary syndrome: Findings from the CCC–ACS project

Key takeaway
This large observational, real–world study of patients from Improving Care for Cardiovascular Disease in China-ACS (CCC-ACS) project, compared the use of ticagrelor vs clopidogrel in ACS patients at high bleeding risk (HBR) and identified that:
- Clopidogrel was prescribed more frequently than ticagrelor
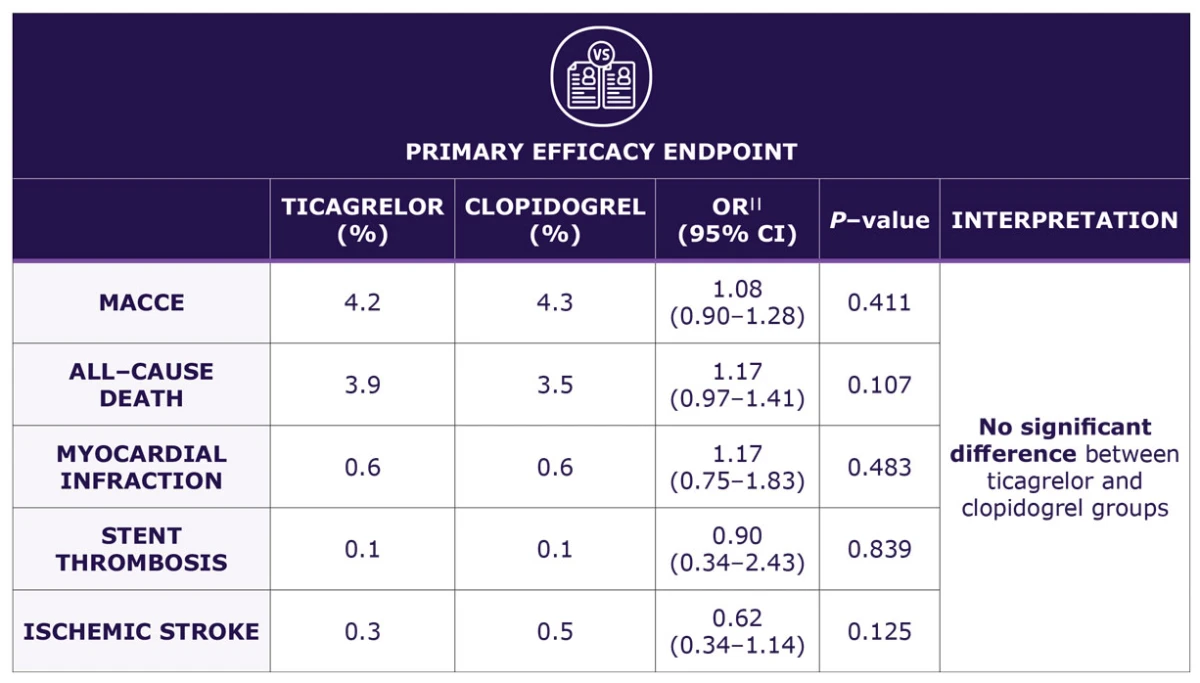
- No significant difference in the risk for in–hospital MACCE between ticagrelor and clopidogrel groups
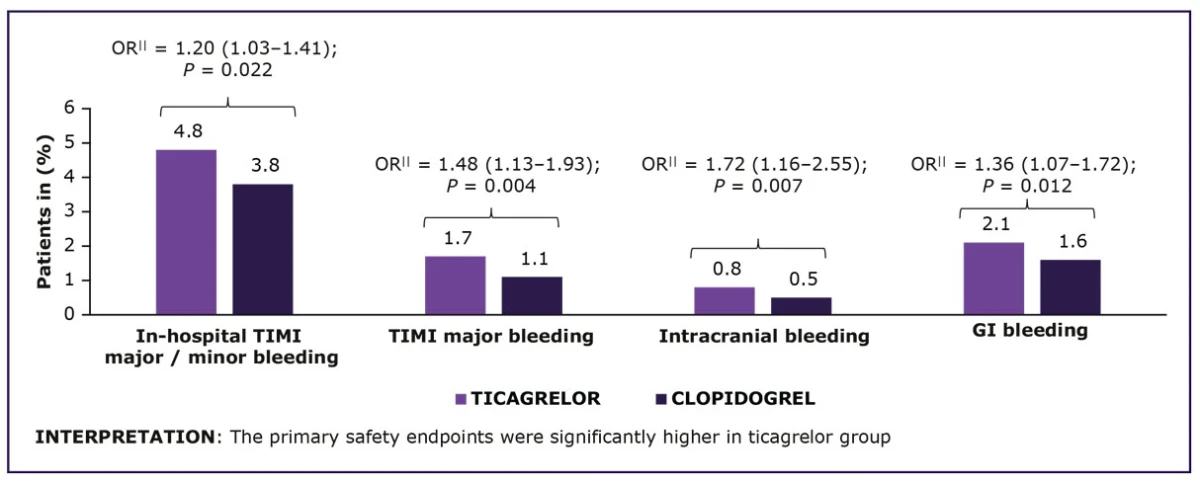
- Ticagrelor* was associated with increase in the rate of in–hospital TIMI major / minor bleeding (by 25%) and in–hospital ICH (by 50%)
− Subgroup analyses showed highest rate of major bleeding with a ticagrelor loading dose - Rates of in–hospital stent thrombosis (ST) and MI were low and similar in both groups, suggesting that clopidogrel might not expose patients to more ischemic risks
Why this matters
Current guidelines recommend ticagrelor over clopidogrel for patients with ACS, regardless of plans for invasive management.
- However, use of guideline recommendations to treat ACS patients at HBR might be challenging due to a higher risk of bleeding events
- Such patients are under–represented / excluded in large clinical trials, resulting in very less clinical evidence to guide optimal choice of a P2Y12 inhibitor
This study evaluated the efficacy and safety of ticagrelor and clopidogrel among real–life ACS patients with HBR during hospitalization.
Study design
- A total of 1,13,650 patients with ACS were registered in CCC–ACS database†
- Patients were divided into non–HBR and HBR groups‡
- 22,120 patients were HBR
- Patients were treated with DAPT§ (aspirin + ticagrelor or clopidogrel)
Key results
Among 22,120 ACS patients categorized as HBR, majority were prescribed clopidogrel (78.8%) and only 21.2% were prescribed ticagrelor.
- BASELINE CHARACTERISTICS: Well balanced between the groups after propensity score matching
- MEDIAN IN–HOSPITAL DURATION: 10 days (IQR = 7–14 days)
Primary Safety Endpoint
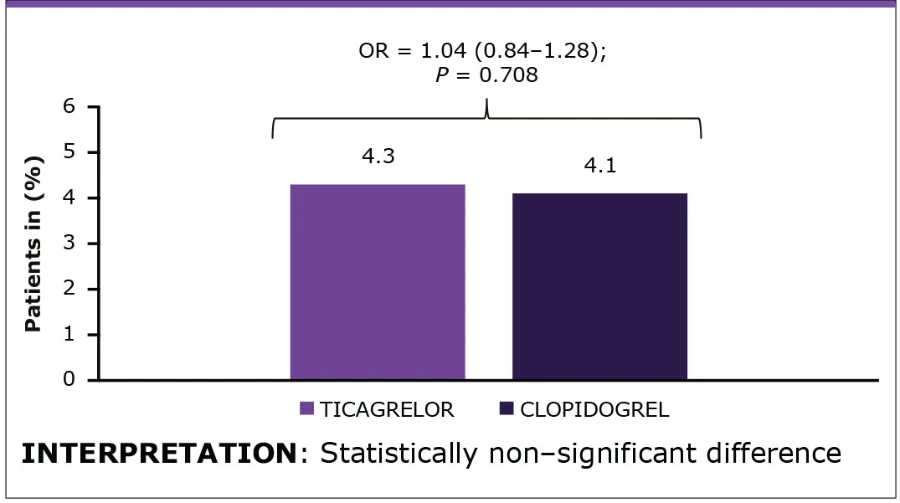
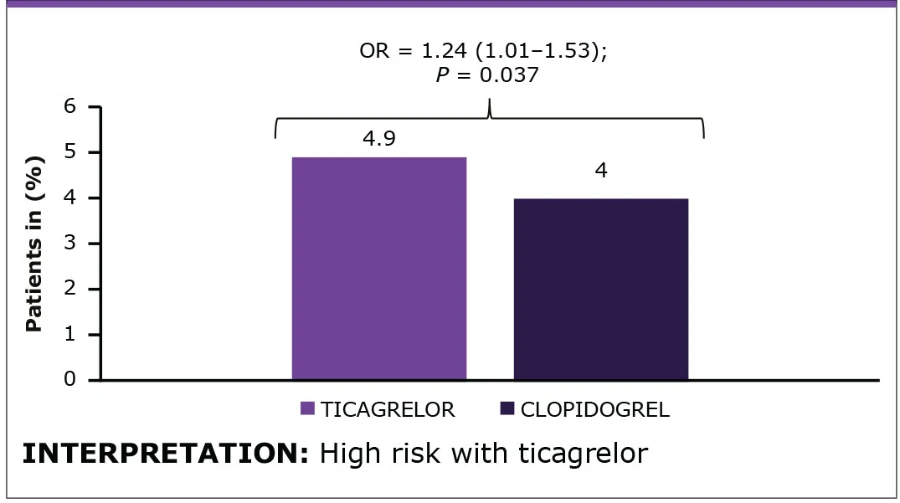
Propensity Scores Matched Cohort: Outcomes consistent with main analysis
In-hospital MACCE
In-hospital TIMI Major / Minor Bleeding
| Parameter | Interpretation |
| In–hospital MACCE | Difference in all subgroup analyse were non-significant |
| In–hospital TIMI major or minor bleeding | Higher risk with ticagrelor treatment observe in patients with hypertension (P = 0.022) and diabetes mellitus (P = 0.040) |
For additional details on CROSS ANALYSIS BY TYPE AND DOSAGE OF P2Y12 INHIBITORS, please click on the hyperlink.
Key limitations
- Only Chinese patients were included in the study; special attention is required while interpreting and expanding the results to Western patients.
- Despite of adjusting for a variety of known variables, unmeasured confounders were still possible.
- HBR was defined accordinng to modified ARC-HBR criteria, which might lead to an underestimation of the prevalence of HBR patients.
- Study focused only on in–hospital outcomes
For additional details, please refer the source publication Wang Y, et al.
* When compared with clopidogrel
† Between 01-NOV-2014 and 30-DEC-2019, from 240 hospitals (Unique identifier: NCT02306616)
‡ According to modified ARC-HBR criteria
§ Without P2Y12 inhibitor cross–over during hospitalization
¶ If any intracranial or fatal bleeding or clinical signs of hemorrhage with Hb: ≥5 g/dL
# Clinical signs of hemorrhage with Hb: 3–5 g/dL
|| Adjusted value
ACS, acute coronary syndrome; ARC-HBR, Academic Research Consortium-HBR; CCC-ACS, improving care for cardiovascular disease in China-ACS; CI, confidence interval; DAPT, dual antiplatelete therapy; GI, gastrointestinal; Hb, hemoglobin; HBR, high bleeding risk; ICH, intracranial hemorrhage; IQR, interquartile range; MI, myocardial infarction; MACCE, major adverse cardiovascular and cerebrovascular event; OR, odds ratio; ST, stent thrombosis; TIMI, thrombolysis in myocardial infarction.
- Wang Y, Yang N, Suo M, Liu X, Wang Z, Zhang X, et al. In–hospital outcomes of ticagrelor versus clopidogrel in high bleeding risk patients with acute coronary syndrome: Findings from the CCC–ACS project. Thromb Res. 2022;216:43–51. doi: 10.1016/j. thromres.2022.04.004. PMID: 35714445.
Interested to know more about our products?
Disclaimer: The images depicted here are fictitious and meant for illustrative purpose only. Any resemblance to any person, living or dead is purely coincidental.



