Bleeding and Clotting: Cancer Therapies That Cause Problems for Patients With Cardiovascular Disease

Key takeaway
Aaron J. Bagnola analyzed the bleeding and clotting risks in cancer and associated therapies in patients with CVD and highlighted the following:1
- There is an increased trend of overlap between cancer and CVD.
- Although risk scores can be helpful, they may not fully capture the risks of bleeding and clotting associated with cancer.
- Specific cancer therapies, such as BTK inhibitors (ibrutinib and ponatinib), are frequently associated with CV toxicities (BP, arrhythmias, and bleeding).
Prophylactic measures are recommended to reduce CV events in cancer patients:1
A multidisciplinary approach is imperative to navigate the complexities of cancer and associated therapies and implement prophylactic measures for risk reduction in patients with CVD.1
Why it matters1
- Despite improvement in High risk survival rate, treatment advances, and early recognition, there is a high risk of CV events in patients with cancer.

- It is crucial to understand these risks, complexities, and potential drug interactions to effectively manage risk reduction in these patients.
Key highlights
- Addition of antiplatelet/anticoagulant therapy: Increased risk of bleeding
- Thrombocytopenia (grade 3–4): 2%–13%
- Low-grade bleeds: ≈50% of patients over 3 years
- Major bleeds (grade 3–4): 4%–8% over a year
Ibrutinib’s association with thrombotic risk, particularly AF:1
- Development of AF: 3%–16%
- Systematic evaluation of 16 separate trials reported an AF incidence of ≈5.77 per 100 person-years in ibrutinib-treated patients.
- Cancer alone increased the thromboembolic risk in patients with AF: The CHA2DS2-VASc score of 1 resulted in a 2-fold increase in HR.
Ibrutinib is associated with AF management:1
Ponatinib’s association with CV events, aoes in particular1
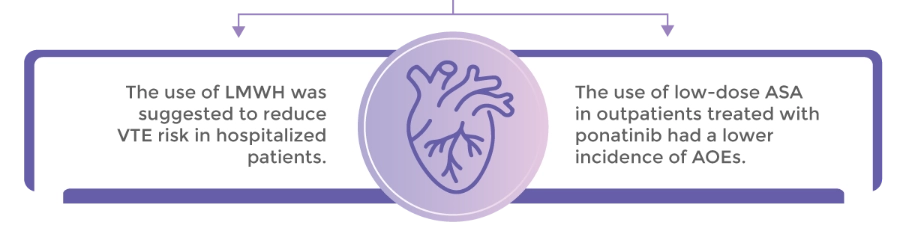
Role of prophylactic measures1
- The use of LMWH was suggested to reduce VTE risk in hospitalized patients with cancer.
- The use of low-dose ASA (100 mg/day) lowered the incidence of AOEs in patients with CML (≥60 years) treated with ponatinib.
Risk stratification using score chart in patients with CML treated with ponatinib:2
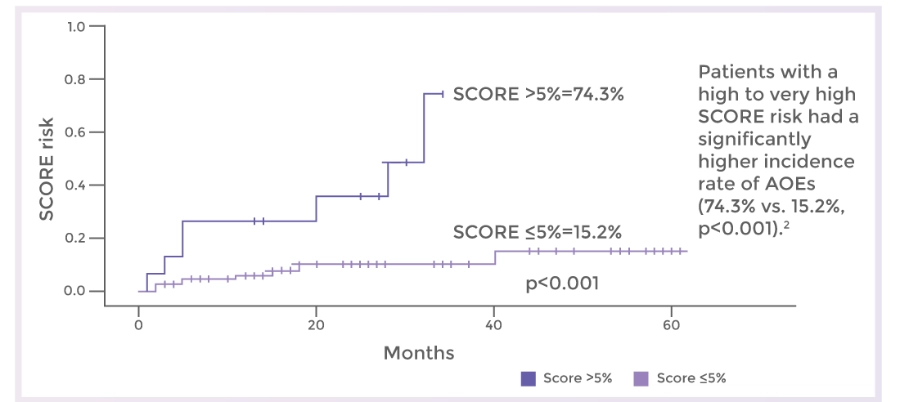
Cumulative incidence of AOEs in patients treated with ponatinib, according to the score risk2
Abbreviations:
AF: Atrial Fibrillation; AOE: Arterial Occlusive Event; ASA: Acetylsalicylic Acid; BP: Blood Pressure; BTK: Bruton Tyrosine Kinase; CCB: Calcium Channel Blocker; CHA2DS2-VASc: Congestive Heart failure, hypertension, age ≥75 years (doubled), diabetes mellitus, prior stroke or transient ischemic attack or thromboembolism (doubled), vascular disease, age 65 to 74 years, sex category (female); CML: Chronic myeloid leukemia; CV: Cardiovascular; CVD: Cardiovascular disease; DOAC: Direct oral anticoagulant; HAS-BLED: Hypertension, abnormal renal/liver function, stroke, bleeding history or predisposition, labile international normalized ratio, elderly (>65 years), drugs/alcohol concomitantly; HR: Hazard ratio; LMWH: Low-molecular–weight heparin; MI: Myocardial infarction; PVD: Peripheral vascular disease; QoL: Quality of life; SCORE: Systematic Coronary Risk Evaluation; VTE: Venous thromboembolism.
- Bagnola AJ. Bleeding and clotting: Cancer therapies that cause problems for patients with cardiovascular disease. Presented at the American College of Cardiology with World Congress of Cardiology (ACC 2023/WCC) on March 05, 2023.
- Caocci G, Mulas O, Abruzzese E, et al. Arterial occlusive events in chronic myeloid leukemia patients treated with ponatinib in the real-life practice are predicted by the Systematic Coronary Risk Evaluation (SCORE) chart. Hematol Oncol. 2019;37(3):296–302.
Disclaimer: For the use of a registered medical practitioner or a hospital or a laboratory only.