Validation of IMPROVE bleeding risk assessment in surgical patients: Insights from DissolVE-2 study

Key takeaway
External validation of IMPROVE BRS to predict the risk of major bleeding* in surgical patients†
of the Chinese cohort (DissolVE 2) demonstrated that:
Improve brs
- Can be implemented for improving both functional and safety outcomes of hospitalized surgical patients
- High predictive accuracy for anticipating major bleeding events in surgical patients
- Favorable AUC for major bleeding events vs any bleeding (major + CRNM‡ bleeding) suggesting better applicability for predicting risk: 0.69 vs 0.55
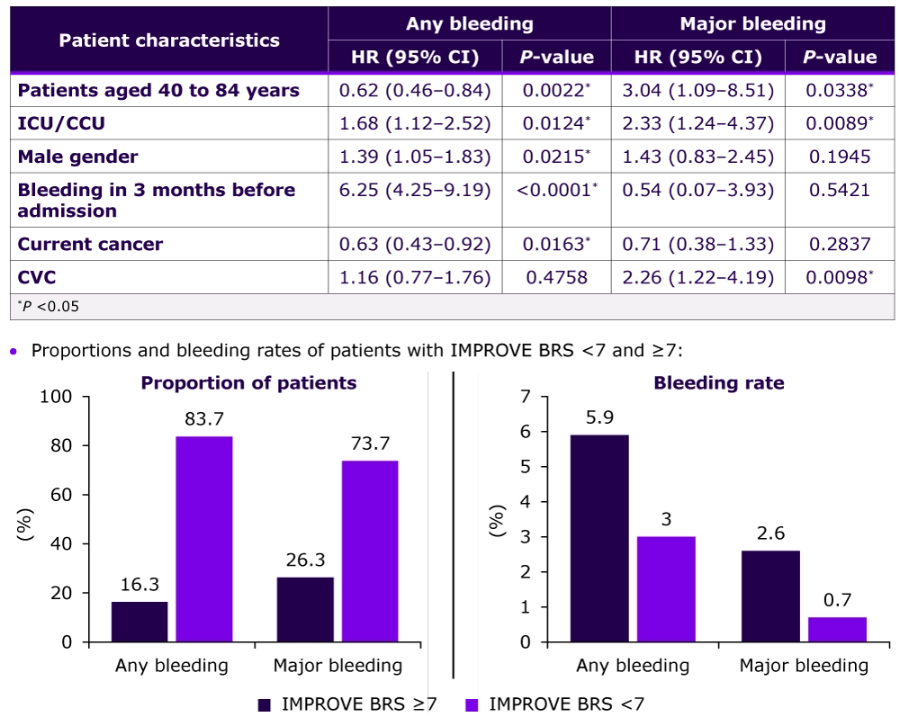
Patients with Improve BRS ≥7
- More likely to experience major bleeding events vs any bleeding (26.3% vs 16.3%)
- Suggesting IMPROVE BRS can effectively differentiate between patients based on bleeding risk
- Suggesting IMPROVE BRS can effectively differentiate between patients based on bleeding risk
- ≈2- to 3-fold increased bleeding incidence vs IMPROVE BRS <7:
- Any bleeding = 5.9% vs 3.0%
- Major bleeding = 2.6% vs 0.7%
Why this matters
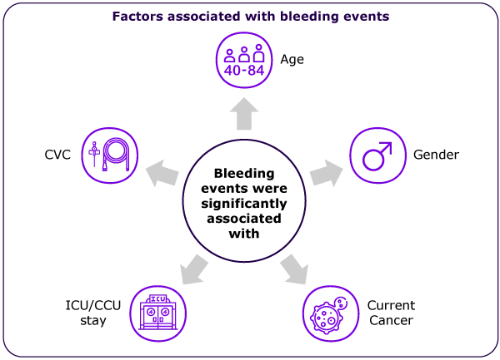
- Bleeding is a major complication in hospitalized surgical patients due to various factors
- Including use of anticoagulants and acquired platelet and hemostatic dysfunctions
- Improve Bleeding RAM is validated in a variety of patient demographics
- However, its applicability to surgical patients has not yet been investigated
This study externally validated IMPROVE BRS in surgical patients to facilitate tailored decisions for the administration of prophylactic or other pre-operative interventions for patients at low-bleeding risk
Study design
Surgical patients of the Chinese cohort from DissolVE-2 study were included,
with an aim to validate IMPROVE BRS
IMPROVE Bleeding RAM
- Consisted of 11 risk factors§ that are individually scored¶, and the total score is calculated for each surgical patient
- Patients are then categorized into two risk groups:
- IMPROVE BRS of <7 = Lower risk of bleeding
- IMPROVE BRS of ≥7 = Higher risk of bleeding
Study outcome
- Occurrence of major bleeding and any bleeding (major + CRNM bleeding) within 14 days of admission

Key Results
Baseline Characteristics
Additional details on the baseline characteristics of patients with major and CRNM bleeding
Cumulative bleeding incidence
- Cumulative incidence of bleeding within 14 days from hospital admission:
- Any bleeding rate = 3.9% (95% CI: 3.4–4.5)
- Of which incidence rate of major bleeding = 1.2% (95% CI: 0.9–1.6)
- Any bleeding rate = 3.9% (95% CI: 3.4–4.5)
Improve brs in surgical patients
Model calibration and discrimination
- Improve BRS showed better predictive accuracy for major bleeding events vs any bleeding (AUC = 0.69 vs 0.55)
Major bleeding
- Excellent goodness of fit (χ2 = 8.44; The Hosmer-Lemeshow test,P = 0.208)
Any bleeding
- Poor goodness of fit (The Hosmer-Lemeshow test, P = 0.004)
Improve BRS had higher AUC (0.83) and better goodness of fit (χ2 = 8.88; P = 0.2616) for major bleeding in patients undergoing abdominal surgery vs other surgery types
Key limitations
- Study is retrospective in nature with no follow-up data
- Bleeding RAM of this study lacks specific surgical factors
Please refer source publication, Zhang Z, et al. for additional details.
*A bleeding event that causes death, clinically severe hemorrhage requiring a blood transfusion of ≥2 units of red blood cells, causing a decrease of hemoglobin levels by ≥2 g/dL, or hemorrhage within a major organ (which includes intraocular, intracranial, pericardial, and retroperitoneal hemorrhage)
† Surgical patients from DissolVE-2 study, who had undergone a surgical operation as per CHEST guidelines (9th edition) and/or were admitted with a major traumatic event not requiring an operation
‡ Hemorrhoid bleeding, epistaxis, or gingival bleeding lasting for >5 min, gross hematuria for >24 h, subcutaneous hematoma for >25 cm2, wound hematoma >100 cm2, hematoma that requires drainage, and other bleeding (which includes clinically overt acute bleeding events important enough to be recorded, for e.g., epistaxis requiring intervention or spontaneous macroscopic hematuria)
§ Age, gender, moderate or severe renal failure, current cancer, rheumatic disease, CVC, ICU/CCU, hepatic failure, platelet count, bleeding in the 3 months before admission, and active gastroduodenal ulcer
¶ Each risk factor is assigned a score ranging from 1 to 4.5 points
Abbreviations:
AUC, area under the curve; BRS, bleeding risk score; CCU, cardiac care unit; CI, confidence interval; CRNM, clinically relevant non major; CVC, central venous catheter; HR, hazard ratio; ICU, intensive care unit; RAM, risk assessment model.
- Zhang Z, Zhen K, Li W, Qin X, Qu J, Shi Y, et al. Validation of the IMPROVE bleeding risk assessment model in surgical patients: Results from the DissolVE-2 study. Thromb Res. 2023;223:69–77. doi: 10.1016/j.thromres.2023.01.013. PMID: 36708692.




