Risk of venous thromboembolism and major bleeding in patients with acute medical illness receiving thromboprophylaxis with enoxaparin
Key takeaway
This large and contemporary population study on patients hospitalized for acute medical illness and initiated enoxaparin prophylaxis in usual clinical setting demonstrated:
- Substantial heterogeneity in risk of VTE and major bleeding (MB)
- Risk stratification might be useful for optimal strategy identification of pharmacological prophylaxis
- Cox model adjusted analyses indicated various risk factors representing baseline conditions prognosticating either an increased risk of symptomatic VTE or MB
- Additional investigations are needed for guiding the clinical practice regarding the optimal strategy of VTE prophylaxis in this population
Why this matters
Patients admitted to hospital with acute medical illness are at an increased risk of VTE events:
- Guidelines recommend adopting an individualized approach to VTE prophylaxis for these patients
- However, there is a paucity of evidence regarding risk stratification within the framework of routine clinical practice
For optimal prophylaxis, assessment of risk of VTE and MB in this population is crucial
This study describes event rates and associated risk factors for VTE and MB along with duration of prophylaxis required in hospitalized acutely ill medical patients receiving thromboprophylaxis with enoxaparin
Study design
Optum database in the USA: Hospitalized patients (≥40 years; between February 2010 to June 2021) for acute medical illness who received enoxaparin prophylaxis
Analysis
- Primary efficacy endpoint: Composite of a new onset symptomatic DVT or PE in either inpatient or outpatient setting*
- Primary safety endpoint: New onset MB event in an inpatient setting*
Assessments
- Cumulative incidence of VTE and MB event rates via 1 − Kaplan-Meier
- Association of baseline conditions with risk of VTE and MB was investigated using Cox proportional hazard model
Key results
Final cohort (patients without AF, CKD, or ongoing antiplatelet or anticoagulation therapy) = 123,022
Key baseline characteristics
| Demographics | Proportion of patients, % | |
| Female | 52.8 | |
| ≥30* BMI, kg/m2 (24 months prior to index) | 36.6 | |
| Clinical condition (within 12 months prior to index) | ||
| History of cancer | 20.5 | |
| History of VTE | 4.5 | |
| History of MB | 1.5 | |
| History of Non-MB | 10.5 | |
| *Represents percent of non-missing values. | ||
Subgroup analysis
| Reasons for hospitalization | ||||
| Subgroups | Percentage of patients,% | Median length of stay, days (IQR) | ||
| Infection | 51.4 | 5 (4–8) | ||
| Respiratory insufficiency | 30.4 | 5 (4–8) | ||
| Cancer | 12.4 | 5 (3–8) | ||
| Ischemic stroke | 9.9 | 4 (3–7) | ||
| Inflammatory condition | 9.4 | 4 (3–7) | ||
| Heart failure | 6.9 | 5 (4–8) | ||
Cancer subgroup: More likely to be younger, female, and have lower prevalence of obesity and pre-existing clinical conditions
Respiratory insufficiency subgroup: More likely to have established COPD vs overall population (45.9% vs 24.7%)
History of VTE: Higher in inflammatory condition subgroup (5.7%), lower in ischemic stroke subgroup (3.3%) vs overall population (4.5%)
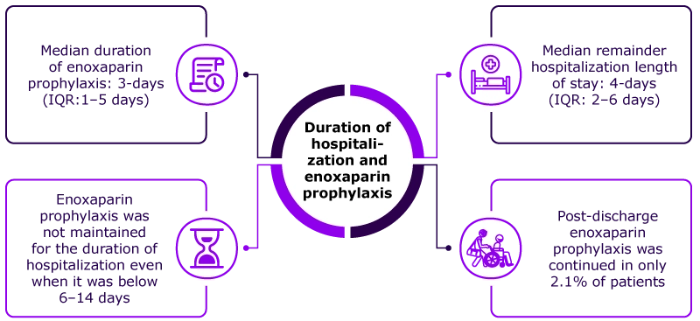
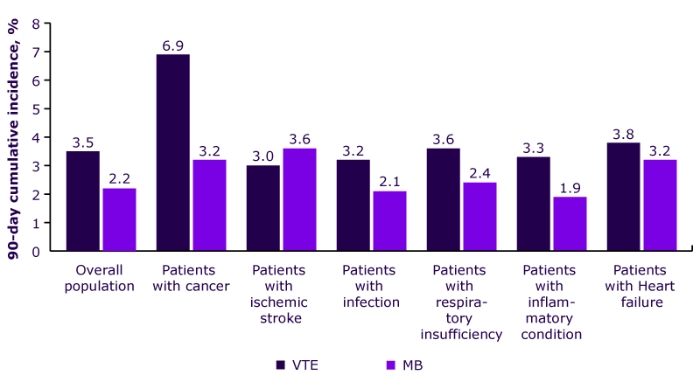
Cumulative incidence of vte and mb
Key factors that increase the risk of vte and mb
| Risk of VTE | HR (95% CI) | |
| VTE History | 4.15 (3.80–4.53) | |
| Hospitalization due to cancer | 2.35 (2.10–2.64) | |
| Thrombophilia | 1.64 (1.29–2.08) | |
| Risk of MB | HR (95% CI) | |
| Non-MB history | 2.46 (2.24–2.70) | |
| Hospitalization due to ischemic stroke | 2.42 (2.11–2.78) | |
| Hospitalization due to cancer | 2.18 (1.88–2.52) | |
| MB history | 2.17 (1.72–2.74) | |
Key strengths
- A large and contemporary population representing usual clinical practice
- Population with well characterized clinical conditions and medications at baseline
- Follow-up was consistent (over 90 days)
- Algorithm was improved for identifying VTE and MB endpoints via codes and other information
Key limitations
- Analysis was based on observational data
- Study included US population covered under a commercial or Medicare Advantage health plan
- Algorithm based identification of VTE, and MB endpoints might lead to misclassification
- Risk factors exhibit patient condition at index† before follow-up
*VTE was defined as symptomatic event in inpatient or outpatient setting. MB was defined as bleeding in a critical area or organ or when bleeding was listed as the primary diagnosis of a hospital stay.
† VTE or MB event in the 90-days prior to index date (the indexdate was defined as the initiation of enoxaparin prophylaxis)
Abbreviations:
AF, atrial fibrillation; BMI, body mass index; CI, confidence interval; COPD, chronic obstructive pulmonary disease; CKD, chronic kidney disease; DVT, deep vein thrombosis; HIV, human immunodeficiency virus; HR, hazard ratio; IQR, interquartile range; MB, major bleeding; PE pulmonary embolism; VTE, venous thromboembolism.
Disclaimer: This content is not intended to supersede or replace any local/ country specific guidance or regulation around cancer-associated thrombosis that would be in place at the time of content generation.
- Le Gal G, et al. Risk of venous thromboembolism and major bleeding in patients with acute medical illness receiving thromboprophylaxis with enoxaparin (Oral presentation: OC 32.2). Presented at the International Society on Thrombosis and Haemostasis (ISTH 2023) congress on June 26, 2023.
Disclaimer: For the use of a registered medical practitioner or a hospital or a laboratory only.




