Venous thromboembolism and major bleeding risk in hospitalized obese patients receiving thromboprophylaxis with enoxaparin

Key takeaways
Prof. Carrier discussed a large cohort study evaluating event rates and risk factors for VTE and major bleeding (MB) in hospitalized obese patients with acute medical illness/surgery receiving enoxaparin prophylaxis*:
Rates of symptomatic VTE in these patients were non-negligible
- Highest event rates were in patients with cancer (7.8%) and those undergoing thoracic surgery
Strongest predictor of VTE:
- History of VTE in both acute medically ill and surgical patients
Highest MB event rates were in:
- Patients with IS (3.7%)
- Patients undergoing thoracic surgery
Strongest predictors of MB:
- Hemorrhagic stroke in acute medically ill patients
- History of MB in surgical patients
Individual risk stratification is needed in these patients to determine the optimal doses and duration of pharmacologic prophylaxis
Why this matters
Hospitalized patients with acute medical illness and those undergoing surgery are at higher risk of developing VTE events
- Obesity is an additional and independent risk factor for VTE in this patient population
Optimal VTE prophylaxis (dose and duration of LMWH therapy) remains uncertain in these obese patients, particularly in morbidly obese patients
This study aimed to evaluate the event rates and risk factors for VTE and MB in obese hospitalized patients with acute medical illness/surgery receiving enoxaparin prophylaxis
Study design
This study included patients from the Optum Market Clarity database† with BMI ≥30 kg/m2 hospitalized with acute medical illness or surgery, who received thromboprophylaxis with enoxaparin
Inclusion criteria
- Age ≥18 years
- One year of continuous enrolment in a health plan before the index date‡
- Initiation of enoxaparin prophylaxis
Exclusion criteria
- VTE, MB, or surgery 90-days prior to index
- Ongoing anticoagulant or DAPT (medication supply within −2, −32 days from index)
- AF, CKD (stages IV and V)§, or dialysis
Assessments
- Cumulative incidences of VTE and MB events (Kaplan-Meier method)
- Risk factors for VTE and MB (Cox proportional hazard models)
Key results
Patients and demographic characteristics
- Overall, 58,186 acute medical illness patients and 30,492 surgical patients met the inclusion criteria; majority of patients were female
Cumulative incidence of vte and mb events by subgroups
Patients with acute medical illness
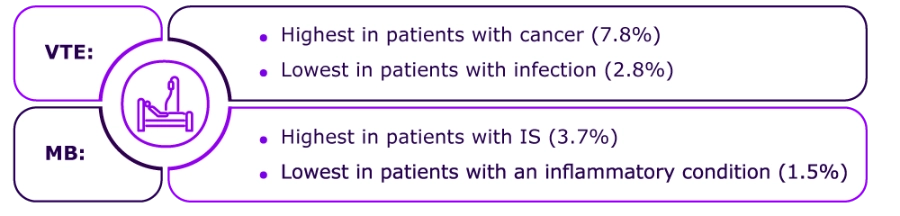
Patients with surgery
Clinical risk factors for vte and mb
VTE: History of VTE was the strongest predictor in both acute medically ill and surgical patients
MB: Hemorrhagic stroke in acute medically ill patients and history of MB in surgical patients were identified as the strongest predictors
Strengths
- Large cohort; contemporary (2010–2021) population were included from usual clinical settings
- These event rates and risk factors may be useful for regulatory authorities, clinicians, payers, and clinical guidelines committees to identify patients at highest risk of adverse events
Limitations
- The study used retrospective data
- Findings were representative of only insured populations in commercial and Medicare Advantage health plans in the USA
*In usual clinical setting
†Represents linked claims and electronic health records information for individuals enrolled in a health plan in the USA
‡The index date was the start of inpatient enoxaparin prophylaxis
§Identified through diagnoses codes or estimated glomerular filtration rate (eGFR)<30
Abbreviations:
AF, atrial fibrillation; BMI, body mass index; CKD, chronic kidney disease; DAPT, dual antiplatelet therapy; IS, ischemic stroke; IQR, interquartile range; LMWH, low-molecular-weight heparins; MB, major bleeding; USA, United States of America; VTE, venous thromboembolism
- Carrier M, et al. Venous thromboembolism and major bleeding risk in hospitalized obese patients receiving thromboprophylaxis with enoxaparin (Poster number: PB1487). Presented at the 31st Congress of the International Society on Thrombosis and Haemostasis (ISTH 2023) on June 27, 2023.
Disclaimer: This content is not intended to supersede or replace any local/country specific guidance or regulation around cancer-associated thrombosis that would be in place at the time of content generation.