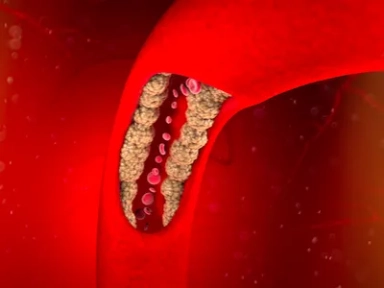
Atherosclerotic Cardiovascular Disease Risk Assessment

Atherosclerotic cardiovascular disease risk assessment: An American Society for Preventive Cardiology clinical practice statement.
The American Society for Preventive Cardiology (ASPC) offers guidance and tools to assess the risk of atherosclerotic cardiovascular disease (ASCVD), with the goal of enabling specialists to provide suitable treatments to prevent ASCVD events.
Key Takeaway
For primary prevention of ASCVD, the first step is to assess cardiovascular risk by determining the global risk score, after which the presence of the following factors can be used to further refine risk estimation:
- Traditional risk factors: Age, sex, diabetes, systolic blood pressure, antihypertensive treatment, total cholesterol, low-density lipoprotein-cholesterol (LDL-C), high-density lipoprotein-cholesterol, and cigarette smoking
- Risk enhancing factors: Family history of premature ASCVD, sex-specific factors, high-risk ethnicities, primary hypercholesterolemia, metabolic syndrome, chronic inflammatory conditions, and chronic kidney disease
- Female-specific factors: Auto-immune disease, menarche, polycystic ovary syndrome, oral contraceptives, infertility, multiparity, adverse pregnancy outcomes, preeclampsia, gestational diabetes mellitus, early menopause, premature ovarian insufficiency, and vasomotor symptoms
- Inflammatory biomarkers: High sensitivity C-reactive protein (hs-CRP), lipoprotein-associated phospholipase A2, myeloperoxidase, myeloid-related protein 8/14, matrix metalloproteinases, lectin-like oxidized LDL receptor-1, and growth differentiation factor-15
- Other biomarkers: Persistently elevated triglycerides, elevated lipoprotein (a) (Lp[a]) or apolipoprotein B, and low ankle-brachial index (ABI)
- Racial / ethnic factors: Non-Hispanic Black, African American, Asian, etc.
- Social determinants of health: Psychological distress, delayed care due to lack of transport, shortage of food, unemployment, lack of health insurance, inability to pay medical bills, or downward social mobility
- Screening for subclinical atherosclerosis:
- Carotid intimal-media thickness or established plaque by carotid ultrasound
- Endothelial function by brachial artery reactivity, large vessel (aorta) or small vessel assessment of vascular health
- Provides the largest decrease in LDL-C with clinical benefits in observational studies.
- Enables early decision on introducing PCSK9 inhibitors.
- Nutritional factors, physical activity, and cardiorespiratory fitness levels play vital roles in ASCVD risk assessment and should also be considered.
- For secondary prevention, risk stratification (very high, high, moderate, or low), followed by immediate and intensive risk factor management are essential.
Why This Matters
- To reduce the risk of developing ASCVD, an accurate assessment of the risk is crucial to provide patients with appropriately targeted preventive therapies.
- Without doing a formal risk assessment, a clinician’s estimate can be inaccurate, which can underestimate the actual risk; hence, the use of global risk scores can be beneficial to improve the application of guideline-based therapies.
- Cardiovascular risk assessment forms the basis of preventive cardiology to determine the appropriateness or intensification of preventive therapy.
Clinical recommendations
- For primary prevention, global risk scoring provides a calculation of ASCVD risk from a set of standard office-based risk factors for a stipulated period.
- Clinicians can then determine the best ways to reduce the risk of developing ASCVD and discuss the same with the patient.
- The presence, number, and / or extent of risk enhancing factors as well as severity of inflammatory factors such as hs-CRP and laboratory measures such as Lp(a) levels can help to further refine treatment decision.
- In women, it is crucial to obtain a complete and thorough reproductive history from menarche to menopause, including premature menopause, preeclampsia, and autoimmune disease.
- Certain race / ethnic groups have a higher risk of developing ASCVD, which can help to further refine the use of preventive therapy.
- Social determinants of health may exert independent effects and should be part of the clinician-patient discussion to determine appropriate ways to lower risk.
- Among screening tests for subclinical ASCVD, CAC testing provides considerable improvement of risk reclassification over global risk scoring in most primary prevention groups, including diabetes.
- Additionally, it can be used to refine decisions on preventive therapy, including on the use of statin and aspirin.
- If CAC scoring is unavailable, carotid ultrasound imaging together with carotid plaque assessment may be beneficial for risk assessment.
- The use of ABI is valuable for assessment of peripheral artery disease and can improve risk reclassification beyond global risk scoring.
- In patients with pre-existing ASCVD, more aggressive treatment should be considered for those at the highest risk, based on the history of either multiple high-risk conditions and one major ASCVD event or multiple major events.
- Patients with recurrent ASCVD events within a short period of time represent an extreme risk for further events
- An even more aggressive risk factor management and intensive treatment should be considered
- Clinician-patient discussions on lifestyle management and on the benefits and risks of evidence-based pharmacologic therapies that are essential to lower the risk of developing ASCVD is central to preventive cardiology.
- Wong ND, Budoff MJ, Ferdinand K, Graham IM, Michos ED, Reddy T, et al. Atherosclerotic cardiovascular disease risk assessment: An American Society for Preventive Cardiology clinical practice statement. Am J Prev Cardiol. 2022;10:100335. doi: 10.1016/j.ajpc.2022.100335. PMID: 35342890.

-from-the-SAFEHEART-registry.png/jcr:content/Clinical%20practice%20experience%20in%20patients%20with%20familial%20hypercholesterolemia%20(FH)%20from%20the%20SAFEHEART%20registry.png)