Key Takeaway
This interim analysis of PERI-DYS study* conducted in Germany compared 1-year outcomes of patients with dyslipidemia and very high CV risk, who received PCSK9i treatment vs those eligible for but did not receive PCSK9i, and showed that:

| Median LDL-C LDL-C at goal <55 mg/dL |
PCSK9i 64.4 mg/dL 40.4% |
No PCSK9i 76.6 mg/dL 21.2% |
| Low achievement of LDL-C goals was due to infrequent LLT intensification |
Why This Matters
- PERI-DYS study compared patients at very high CV risk treated with PCSK9i vs those eligible for but did not receive PCSK9i, exploring differences and subsequent treatment patterns
- Interim analysis reported changes in LDL-C levels and factors associated with treatment intensification 12 months after patient enrollment

Study Design
STUDY TYPE
- Prospective, open-label, noninterventional study (NCT03110432; at 70 sites in Germany)
STUDY POPULATION
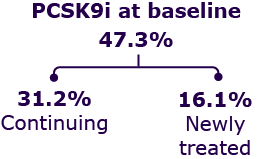
- Patients with dyslipidemia and very high CV risk (N = 1,713)
Key Results
Mean age
63.4 years (± 11.5)
Sex
35% women
Baseline characteristics
| Parameter | PCSK9i (n = 810) |
No PCSK9i (n = 903) |
| Age, years | 62 ± 10 | 64 ± 12 |
| CHD, % | 74 | 68 |
| Untreated LDL-C, mg/dL | 201 | 179 |
| Statin intolerance, % | 67.3 | 15.3 |
Patients treated with PCSK9i vs not treated with PCSK9i were:
- Younger
- More likely to have:
– CHD
– Higher untreated LDL-C
– Statin intolerance
Median LDL-C at 1 year:
PCSK9i vs no PCSK9i

Lower median LDL-C level was seen in patients on PCSK9i vs those not on PCSK9i
LDL-C at goal <55 mg/dL
at 1 year: PCSK9i vs no PCSK9i

LDL-C at goal <55 mg/dL in more patients on PCSK9i vs those not on PCSK9i
LDL-C (<55 mg/dL) goal achievement in patients receiving PCSK9i + statin
at baseline vs PCSK9i only vs statin only at 1 year

Patients on PCSK9i + statin at baseline showed highest LDL-C goal achievement (<55 mg/dL) vs patients only on PCSK9i or only on statin
Proportion of patients having unchanged LLT
vs those having modified therapy at 1 year

| PATIENTS WITH MODIFIED THERAPY | ||
| PCSK9i | No PCSK9i | |
| Intensification of therapy | 7% | 19% |
| PCSK9i Add-on Discontinuation |
0% 6% |
4% 0% |
| Statin Add-on Discontinuation |
4% 3% |
3% 4% |
| Statin intensity increase | 2% | 8% |
| Ezetimibe Add-on Discontinuation |
3% 4% |
7% 3% |
Results from multivariate model
High LDL-C (e.g., 100–119 mg/dL) was significantly associated with LLT intensification (OR = 2.3)
Conversely, following were statistically significant factors with less likelihood for LLT intensification:

Older age
60+ years; OR = 0.7

Ezetimibe at baseline
OR = 0.7

Statin intolerance at baseline
OR = 0.7
*Prospective, open-label, non-interventional.
ABBREVIATIONS:
CHD, coronary heart disease; CV, cardiovascular; LDL-C, low-density lipoprotein-cholesterol; LLT, lipid-lowering therapy; OR, odds ratio; PCSK9, proprotein convertase subtilisin/kexin type 9; PCSK9i, protein convertase subtilisin/kexin type 9 inhibitor.
Parhofer KG, et al. Management of patients with very high cardiovascular risk eligible for PCSK9 inhibitor treatment: 1-year outcomes of the PERI-DYS study (Poster number: SS119/#332). Presented at the 91st European Atherosclerosis Society Congress (EAS 2023) on May 23, 2023.
MAT-KW-2300338/V1/OCT2023