Maternal and perinatal outcomes of venous thromboembolism in high-risk cohort using a multidisciplinary treatment approach
Adapted from Ernst DM et al. Int J Gynecol Obstet. 2021;154(3): 500–507.

Key Takeaway
- Perinatal surveillance of pregnant women with a high-risk of VTE should include guided thromboprophylaxis and close observation to decrease perinatal risk
- Multidisciplinary assessment of VTE in high-risk pregnant women should be supported
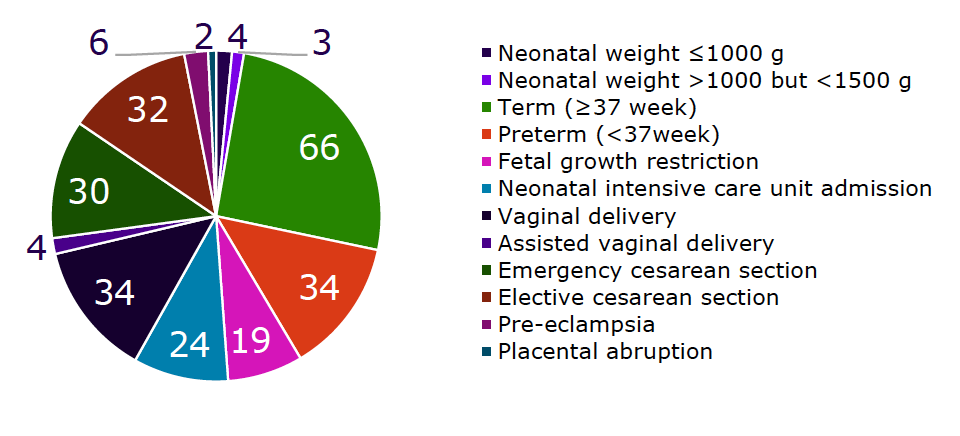
- Women at high risk of thrombosis during pregnancy are at high risk of pre-eclampsia, preterm delivery, and growth restriction
Why This Matters
- Pregnant women are at >4 times higher risk of VTE compared with nonpregnant women1
- Thromboprophylaxis in these patients is guided by a low level of evidence due to limited data from RCT2,3
- Risk of VTE is five-fold higher during puerperium
- An alternative approach in these patients is development of protocols for risk stratification and pharmacological thromboprophylaxis

Study Design
A cohort of pregnant women prospectively referred to the multidisciplinary clinic of the Maternal-Fetal Group of the Red de Salud UC-Christus for a high risk of VTE between January 1, 2007 to December 31, 2019 were analyzed
Inclusion criteria
All pregnant women
Exclusion criteria
Women seeking preconception advice regarding the risk of VTE who did not become pregnant during the period of the analysis
A modified diagnostic workup algorithm and a therapeutic algorithm were developed based on consensus guidelines
Key Results
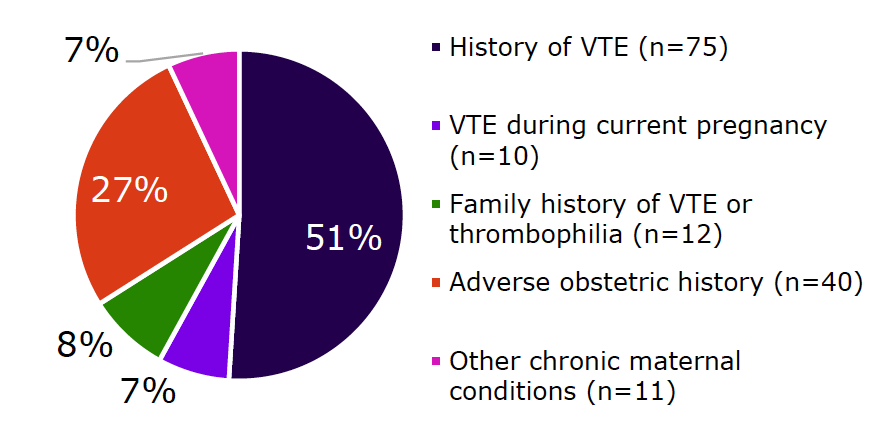
Patient population
- Total of 148 pregnancies included
- Median age: 32 years, 26% patients >35 years
Clinical characteristics
- High risk VTE: 57% (n=85)
Diagnostic workup
- Thrombophilia: 57% (n=85)
- Most common thrombophilia was APS (34%; n=29), more frequent in women with obstetric conditions than with prior VTE episodes
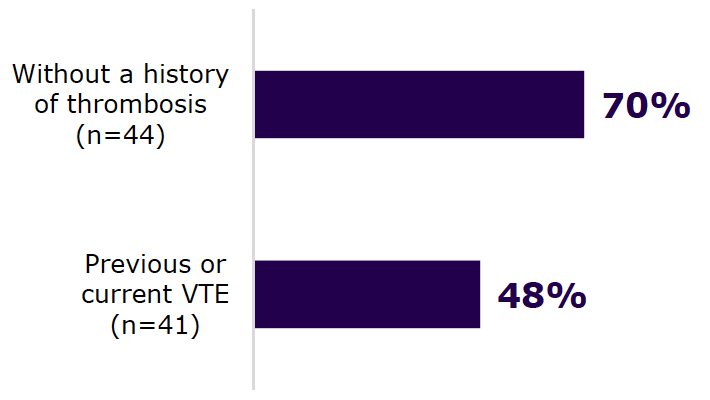
ASA and LMWH therapy
- VTE under prophylactic or therapeutic treatment was 0% during pregnancy and 3% during puerperium
Perinatal outcomes
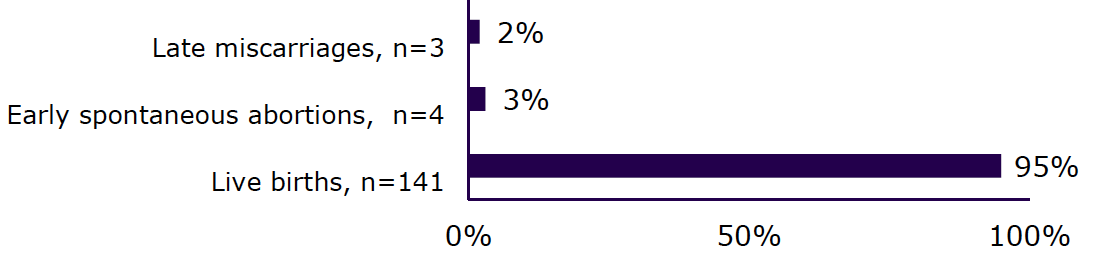
Obstetric complications among live births (%)
Limitations
- Study design does not indicate if the chosen treatment management option was better than other alternatives
- Lack of control group (due to ethical reasons)
- Additional efforts are warranted to decrease perinatal risk
ABBREVIATIONS
ASA, acetylsalicylic acid; APS, antiphospholipid syndrome; LMWH, low molecular weight heparin; VTE, venous thromboembolism.
- Heit JA, Kobbervig CE, James AH, Petterson TM, Bailey KR, Melton LJ 3rd. Trends in the incidence of venous thromboembolism during pregnancy or postpartum: a 30-year population-based study. Ann Intern Med. 2005;143(10):697-706.
- Bates SM, Rajasekhar A, Middeldorp S, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: venous thromboembolism in the context of pregnancy. Blood Adv. 2018;2(22):3317-3359.
- Palmerola KL, D'Alton ME, Brock CO, Friedman AM. A comparison of recommendations for pharmacologic thromboembolism prophylaxis after caesarean delivery from three major guidelines. BJOG. 2016;123(13):2157-2162.
MAT-BH-2300442/V1/June2023