Ticagrelor vs Clopidogrel in ACS patients undergoing PCI in routine clinical practice

Main Takeaway
- Risk for net adverse clinical events (NACE) was not significantly different between ticagrelor at 12 months compared with clopidogrel
- Study population: 62,580 patients with acute coronary syndrome (ACS) who underwent percutaneous coronary intervention (PCI) in routine clinical practice
- Ticagrelor was associated with higher risks for haemorrhagic events and dyspnoea vs clopidogrel
Why This Matters
- Recent observational studies question whether ticagrelor vs clopidogrel is associated with better outcomes in routine clinical practice
- Current guidelines: recommend ticagrelor with aspirin in preference to clopidogrel in patients with ACS
Study Design
Retrospective cohort study: 183,579 patients (age range, 30-89 years) with ACS who underwent PCI and received ticagrelor or clopidogrel
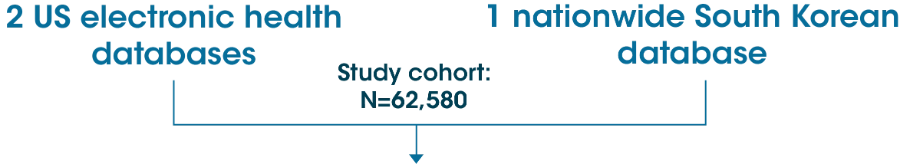
Patients were matched using propensity score:
- Ticagrelor (n=31,290)
- Clopidogrel (n=31,290)
Primary endpoint: NACE at 12 months
- Ischaemic events
[recurrent acute myocardial infarction, revascularisation or ischaemic stroke] - Haemorrhagic events
[haemorrhagic stroke or gastrointestinal bleeding]
Secondary outcomes: NACE or mortality, all-cause mortality, composite ischaemic events, composite haemorrhagic events, individual components of the primary outcome, dyspnoea at 12 months
Key Results
95.5% of matched patients used aspirin with ticagrelor or clopidogrel among the 31,290 propensity-matched pairs
The risk for NACE was not significantly different between ticagrelor and clopidogrel groups (HR, 1.05; 95% CI, 1.00-1.10; P=0.06)
- No significant difference was found between the 2 groups for:
- NACE or mortality (HR, 1.03; 95% CI, 0.98-1.08; P=0.21)
- Ischaemic events (HR, 1.03; 95% CI, 0.98-1.08; P=0.32)
- All-cause mortality (HR, 0.97; 95% CI, 0.81-1.16; P=0.74)
- Ticagrelor vs clopidogrel group showed a significantly higher risk for:
- Haemorrhagic events (HR, 1.35; 95% CI, 1.13-1.61; P=0.001)
- Dyspnoea (HR, 1.21; 95% CI, 1.17-1.26; P<0.001)
Limitations
- The study did not include information on aspirin dosage, angiographic findings, or PCI procedure
- The burden of overall bleeding events could have been underestimated or overestimated
- Neither the proportion of patients who switched antiplatelet drugs nor its effects were quantified
- The effect of pre-treatment with an antiplatelet agent was not assessed
- The mortality rate might have been underestimated
- Patients who used prasugrel for dual antiplatelet therapy were not included
- You SC et al. Association of Ticagrelor vs Clopidogrel With Net Adverse Clinical Events in Patients With Acute Coronary Syndrome Undergoing Percutaneous Coronary Intervention. JAMA. 2020;324(16):1640-1650. doi:10.1001/jama.2020.16167.