Consensus Guidance for Monitoring Children with Islet Autoantibody-Positive Pre-Stage 3 Autoimmune Type 1 Diabetes (T1D)

Screening and monitoring are critical to managing autoimmune T1D and reducing the likelihood of diabetic ketoacidosis (DKA) hospitalization or emergency care at the time of Stage 3 autoimmune T1D diagnosis.1
Testing for islet autoantibodies against four major pancreatic autoantigens is currently available:
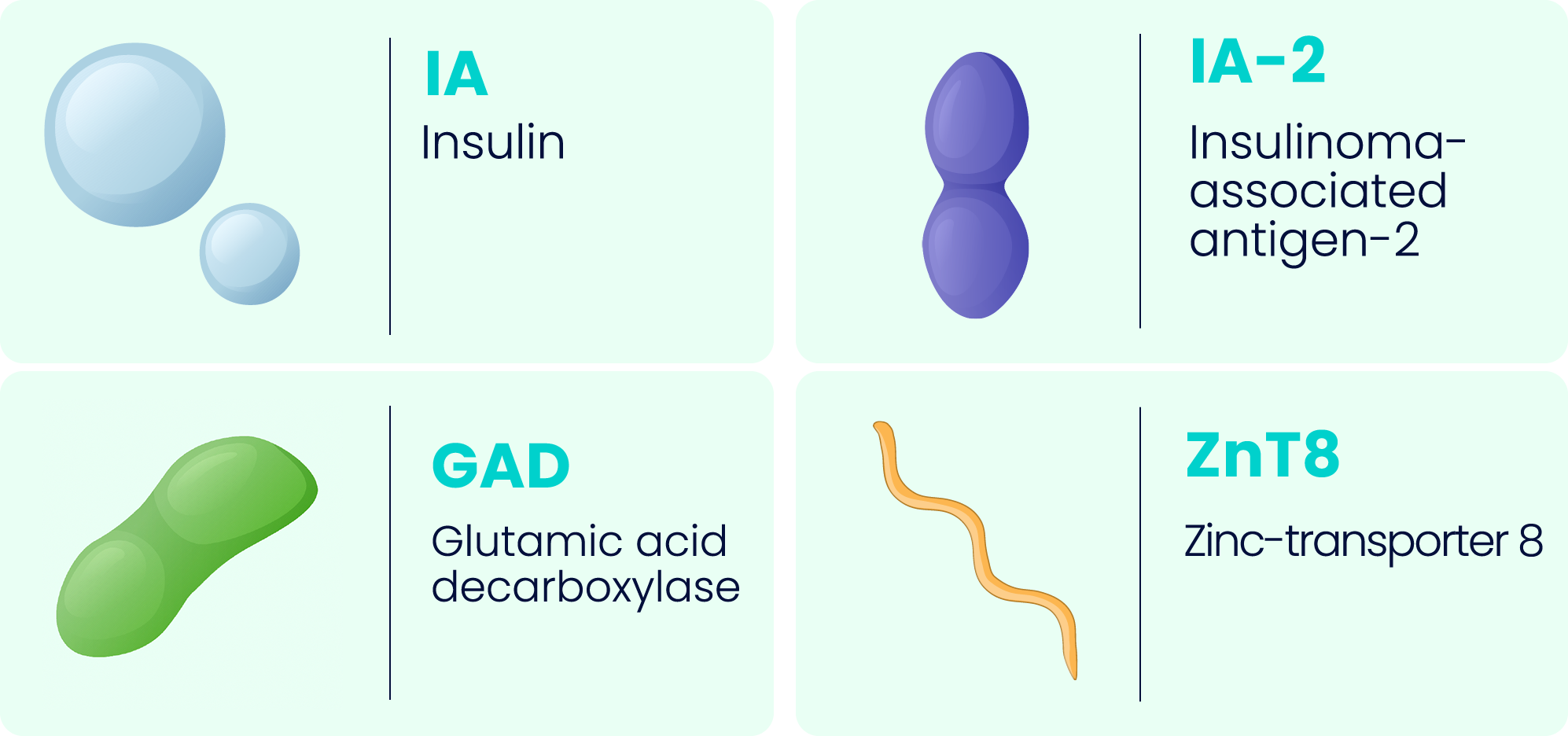
A combination of these four primary types of autoantibodies is recommended to detect autoimmunity.1-3
The presence of islet autoantibodies alongside metabolic status defines the three stages of T1D.4
These screening criteria are recommended by the most recent ADA Standards of Care.1
At-risk ≤1 autoantibody
Normoglycemia
How to confirm single IAb+ status1
| CONFIRM RESULTS | |
 | After first detection of single IAb, follow the ‘rule of twos’, using two independent methods to confirm negative results for other IAbs.1 |
| MONITORING FREQUENCY (children <3 years old) | |
 | Monitor IAb+ status every 6 months for 3 years, then annually thereafter for 3 more years.1 |
 | Metabolic monitoring includes random venous or capillary blood glucose and HbA1c values at the same frequency.1 |
 | If no progression, stop autoantibody and metabolic monitoring and counsel for risk of clinical disease.1 |
| MONITORING FREQUENCY (children ≥3 years old) | |
 | Monitor IAb+ status annually for 3 years.1 |
 | Metabolic monitoring includes annual random venous or capillary blood glucose and HbA1c testing for 3 years.1 |
 | If no progression, stop autoantibody and metabolic monitoring and counsel for risk of clinical disease.1 |
 | Critical monitoring during early years
|
Stage 1 (early stage) ≥2 autoantibodies
Normoglycemia
How to confirm multiple IAb+ status1
| CONFIRM RESULTS | |
 | After first detection of ≥2 IAbs, follow the ‘rule of twos’, using two independent methods to confirm positive status for other islet autoantibodies.1 |
 | TWO-TEST CONFIRMATION NOT POSSIBLE? A single blood test positive for multiple islet autoantibody status identifies a person with sufficient risk for metabolic monitoring.1 |
 | REVERTED STATUS? For adults with previously confirmed multiple IAb+ status who revert to single IAb+ or IAb− status, metabolic monitoring should follow the guidelines below for Stage 1.1 |
GENERAL GUIDELINES FOR METABOLIC MONITORING1
| <3 years old Once every 3 months1 | 3–9 years old At least every 6 months1 | >9 years old At least every 12 months1 |
 | Conduct monitoring based on staging criteria and modalities described in Tables 1 and 5 of the consensus guidelines.1 |
 | Ensure monitoring is done when the child is healthy and not experiencing intercurrent illness.1 |
 | Provide SMBG meters and strips to all children with multiple islet autoantibody positivity or their parents.1 |
 | During intercurrent illness (e.g., a cold), use SMBG to detect hyperglycemia.1 |
 | For recent confirmation of multiple IAb+ status, perform SMBG tests on two different days over a 2-week period, then once every 1–3 months.1 |
Stage 2 (early stage) ≥2 autoantibodies
Glucose intolerance or dysglycemia
How to confirm multiple IAb+ status1
| CONFIRM RESULTS1 | |
 | After first detection of ≥2 IAbs, follow the ‘rule of twos’, using two independent methods to confirm positive status for other islet autoantibodies.1 |
 | TWO-TEST CONFIRMATION NOT POSSIBLE? A single blood test positive for multiple islet autoantibody status identifies a person with sufficient risk for metabolic monitoring.1 |
 | REVERTED STATUS? For adults with previously confirmed multiple IAb+ status who revert to single IAb+ or IAb− status, metabolic monitoring should follow the guidelines below for Stage 2.1 |
GENERAL GUIDELINES FOR METABOLIC MONITORING1
 | Monitor measures of glucose regulation (glycemic status) every 3 months. |
 | A longitudinal change in HbA1c of ≥10% from the confirmed islet autoantibody date may indicate dysglycemia and disease progression.1 |
 | Perform an OGTT to assess T1D stage for therapy eligibility.1 |
 | Measure random venous or capillary blood glucose simultaneously with HbA1c.1 |
 | Use 10–14-day CGM periodically at a similar frequency as HbA1c measurement.1 |
 | Monitor objective weight trends using a growth chart and ensure a healthy meal plan to preclude disordered eating behaviors as a cause of weight change.1 |
 | OGTT is the established gold standard to classify Stage 1, Stage 2 or Stage 3 T1D however if OGTT is not possible:1
|
| CGM usage | |
 | CGM should be blinded to the individual and interpreted by trained HCPs.1 |
 | Criteria for CGM metrics to diagnose Stage 2 or Stage 3 T1D require further research.1 |
All persons at risk through to Stage 2
PSYCHOSOCIAL SUPPORT FOR SINGLE AND MULTIPLE IAb+ INDIVIDUALS
 | Emotional, cognitive and behavioral functioning should be assessed in people at risk of or with early-stage autoimmune type 1 diabetes and their family members, when appropriate. Anxiety, risk perception and behavior changes should specifically be assessed.1 |
 | Ask the individual at risk or with early-stage type 1 diabetes and/or their caregivers and family members about their reactions upon receiving the news that they have type 1 diabetes-related autoantibodies. This can be accomplished using guiding questions and standardized and validated questionnaires.1 |
 | At each monitoring visit, there should be enquiries into current needs, particularly coping.1 |
 | Psychological care should be integrated into routine medical visits and, whenever possible, delivered by providers with diabetes-specific training.1 |
Stage 3 ≥1 autoantibodies
Persistent hyperglycemia with or without symptoms
Screening and subsequent monitoring for presymptomatic T1D prior to clinical onset of Stage 3 have several benefits, including reducing the risk of DKA and hospitalization, and providing opportunities for education and preparation for chronic disease management.5,6
The decision to start insulin depends on a range of factors and consideration to do so should be referred to a specialist center.1
For the full guidelines together with the evidence rating (A–E), please consult reference 1.
ADA, American Diabetes Association; CGM, continuous glucose monitoring; DKA, diabetic ketoacidosis; GAD, glutamic acid decarboxylase; HbA1c, glycated hemoglobin; HCP, healthcare professional; IA-2, insulinoma-associated antigen-2; IAA, insulin autoantibody; IAb, islet autoantibody; OGTT, oral glucose tolerance test; SMBG, self-monitoring of blood glucose; T1D, type 1 diabetes; T2D, type 2 diabetes; ZnT8, zinc-transporter 8.
- Phillip M, et al. Diabetes Care. 2024;47(8):1276-98.
- Winter WE, et al. J Appl Lab Med. 2022;7:197-205.
- Peters A. J Fam Pract. 2021;20; Suppl:S47-S52.
- Insel RA, et al. Diabetes Care. 2015;38(10):1964-74.
- Besser REJ, et al. Arch Dis Child. 2022;107(9):790-5.
- Hendriks AEJ, et al. Diabetes Metabl Res Rev. 2024;40(2):e3777.