{
event: "article_read",
name: `Effect of de-escalated P2Y12 inhibitor switching in dual antiplatelet therapy (DAPT)`,
author: ``,
tags: `Cardiovascular | Atherothrombosis`,
publication_date: ``,
interaction_type: "content"
}
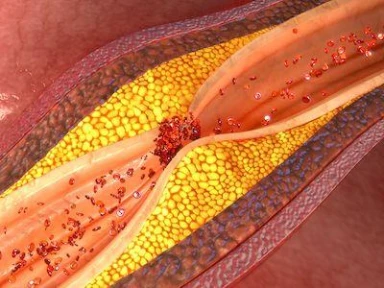
Effect of de-escalated P2Y12 inhibitor switching in dual antiplatelet therapy (DAPT)
Main Takeaway
A real-word study of Taiwanese patients with AMI undergoing PCI
- Showed a comparable 1-year cardiovascular outcome with standard ticagrelor treatment 3 months after the event of AMI
- Didn’t report statistically significant differences in:
- Hazard risk of death
- AMI admission
- Major adverse
- Cardiovascular events (MACE)
- Didn’t show a difference in the risk of bleeding, including major or clinically relevant non-major bleeding
Why This Matters
- Bleeding risks could be reduced P2Y12 inhibitor de-escalation approach is considered by physicians to reduce additional bleeding risks
- Current studies are not enough Despite recent clinical studies, there’s limited and conflicting evidence on de-escalation strategies. This study aimed to assess the effect of de-escalated P2Y12 inhibitor switching in DAPT on MACE in patients with AMI undergoing PCI;
Study Design
This retrospective and population-based cohort study utilized data from the Taiwan’s National Health Insurance Research Database (NHIRD).
Key Inclusion Criteria:
- Patients who were hospitalized with a primary diagnosis of AMI
Key Exclusion Criteria:
- Patients aged <18 years, without identification of sex, or Taiwanese citizenship
- Patients not on heparin or antiplatelet therapy, or were only on aspirin therapy, or
- received antiplatelet agents other than ticagrelor at index of AMI
- Patients who had a coronary artery bypass graft
- Death of the patient within 3 months after the index date of AMI
Key Outcomes:
- Death, AMI readmission, and MACE within one year during the follow-up period
Key Results
Number Of Participants
- 10,100 patients were included (de-escalated DAPT group: n = 1,901; unchanged DAPT: n = 8,199)
Incidence Rates And Adjusted Hazard Ratio
- All-cause death (unchanged vs de-escalated DAPT group): Incidence = 2.42 (95% confidence interval [CI]: 2.02–2.90) vs 2.89 (95% CI: 2.05–3.91); adjusted HR = 1.20 (95% CI: 0.83–1.73; P = 0.336)
- AMI hospitalization (unchanged vs de-escalated DAPT group): Incidence = 3.28 (95% CI: 2.81–3.83) vs 3.68 (95% CI: 2.75–4.88); adjusted HR = 1.12 (95% CI: 0.80–1.56; P = 0.509)
- MACE (unchanged vs de-escalated DAPT group): Incidence = 4.72 (95% CI: 4.13–5.36) vs 4.91 (95% CI: 3.80–6.26); adjusted HR = 1.04 (95% CI: 0.78–1.39; P = 0.766)
- Major bleeding (unchanged vs de-escalated DAPT group): Incidence = 2.36 (95% CI: 1.95–2.82) vs 2.12 (95% CI: 1.41–3.01); adjusted HR = 0.92 (95% CI: 0.61–1.37; P = 0.669)
Limitations
- Patient information such as risk behaviors, diet, and physical activities are not available in the NHIRD.
- Hidden bias of medication selection was introduced as the study data was sourced from an administrative database.
- Missing clinical information, such as the severity of AMI at admission, might have induced non-differential misclassification bias.
- Study results might not be generalizable to other populations, as only Taiwanese patients were included in the analysis.
- Yeh JS, Hsu CY, Huang CY, Chen WT, Hsieh YC, Chien LN. The effect of de-escalation of P2Y12 receptor inhibitor therapy after acute myocardial infarction in patients undergoing percutaneous coronary intervention: A nationwide cohort study. PLoS One. 2021;16(1):e0246029. doi: 10.1371/journal.pone.0246029. PMID: 33493236.
Related articles
MAT-BH-2200185/v2/Jun 2023


.webp/jcr:content/jcr_content%20(3).webp)