UNDERSTANDING
GM2 GANGLIOSIDOSES
GM2 gangliosidoses comprise rare, neurodegenerative lysosomal storage disorders, primarily Tay-Sachs disease and Sandhoff disease, caused by deficiency of β-hexosaminidase.
Accumulation of GM2 occurs primarily within neurons and progressively destroys nerve cells in the brain and spinal cord, leading to neurodegenerative symptoms.1,2,3
Zoe,
Living with GM2 gangliosidoses,
USA
Late-onset forms of the disease include debilitating and progressive proximal muscle weakness and imbalance.18

|
Clinical subtypes of GM2 gangliosidoses10,13-15 Subtypes of GM2 gangliosidoses are categorized according to age at onset. |
||
|
Infantile form is aggressive and leads to premature death at approximately 4 years of age |
Death is likely mid-to late-teens |
Variable clinical course and life expectancy |
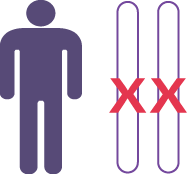
GENETIC PROFILE
GM2 gangliosidoses are inherited in an autosomal recessive manner. If both parents are carriers of the disease-causing allele, their child has a 25% chance of being affected.
Males and females have an equal chance of being affected.17
IMPORTANCE OF EARLY DIAGNOSIS
The average time from symptom onset to diagnosis for late-onset GM2 gangliosidoses is 16 years. The large delay in diagnosis is due in part to the nonspecific nature of early symptoms and lack of disease awareness. GM2 gangliosidoses are progressive and can lead to irreversible damage to major body organs.18
 |
HOW TO DIAGNOSE |
Diagnosis of GM2 gangliosidoses can be accomplished by measurement of Hex A or Hex B enzyme activity.

Confirmatory diagnosis is recommended by detection of two pathogenic variants in HEXA or HEXB .16
|
INCIDENCE AND HIGH-RISK POPULATIONS Incidence is likely to be underestimated due to misdiagnosis and delayed diagnosis resulting from limited disease awareness.4-12 |
 |
 |
||
| Incidence | Carrier frequency | High risk populations | |
| Tay-Sachs disease |
|
|
|
| Sandhoff disease |
|
|
GM2 gangliosidoses display a broad range of manifestations, and the similarity with other diseases highlights the importance of confirmatory diagnosis
| Primary symptoms | GM2 gangliosidoses | Spinocerebellar ataxia (SCA) | Spinal muscular atrophy (SMA) | Amyotrophic lateral sclerosis (ALS) |
| Impaired cognitive function | ● | |||
| Psychiatric abnormalities | ● | |||
| Psychomotor deterioration | ● | ● | ||
| Dysphagia | ● | ● | ● | |
| Dysarthria | ● | ● | ● | |
| Visual problems | ● | ● | ||
| Retinal cherry-red spot | ● | |||
| Seizures | ● | |||
| Balance issues | ● | |||
| Ataxia | ● | ● | ● | |
| Dysmetria | ● | ● | ● | |
| Spasticity | ● | ● | ||
| Myoclonus | ● | |||
| Abnormal posture | ● | |||
| Atrophy/muscle weakness | ● | ● | ● | |
| Proximal muscle weakness presenting as symmetric and clinically predominant in the psoas, triceps and interosseus muscles | ● |
x |
||
| Pyramidal syndrome | ● |
x |
||
| Bulbar lower motor neuron disorder and evolution |
x |
● | ||
| Dyspnea | ● | ● |
● Symptom often observed with the disease
x Symptom not associated with the disease
Masingue M et al. Ann Neurol. 2020;87:609; Neudorfer et al. Genet Med. 2005;7:119; Regier DS et al. Pediatr Endocrinol Rev. 2016;13:663; Bley AE et al. Pediatrics. 2011;128:e1233; Bao Y et al. J Neurol Res. 2019;9:81; Kolb SJ and Kissel JT. Neurol Clin. 2015;33:831; Chen S et al. Mol Neurodegener. 2013;8:28.
- Neudorfer O et al. Genet Med. 2005;7:119.
- Regier DS et al. Pediatr Endocrinol Rev. 2016;13:663.
- Leal AF et al. Int J Mol Sci. 2020;21:6213.
- Triggs-Raine BL et al. New Engl J Med. 1990;323:6.
- Triggs-Raine BL et al. Am J Hum Genet. 1995;56:870.
- Vallance H and Ford J. Crit Rev Clin Lab Sci. 2003;40:473.
- Frey LC et al. JAMA Neurol. 2005;62:989.
- Neudorfer O et al. Genet Med. 2005;7:119.
- Maegawa GHB et al. Pediatrics. 2006;118:e1550.
- Bley AE et al. Pediatrics. 2011;128:e1233.
- Kaback MM and Desnick RJ. Gene Reviews: Hexosaminidase A deficiency. 2011.
- Lew RM et al. Appl Clin Genet. 2015;8:19.
- Jeyakumar M et al. Neuropath Appl Neurobiol. 2002;28:343.
- Bley AE et al. Pediatrics. 2011;128:e1233.
- Kaback MM and Desnick RJ. Gene Reviews: Hexosaminidase A deficiency. 2011.
- Leal AF et al. Int J Mol Sci. 2020;21:6213.
- Cachon-Gonzalez MB, et al. Curr Gene Ther. 2018;18(2):68-89.
- Toro C et al. Neurosci Lett. 2021 Nov 1;764:136195.
MAT-KW-2400091-V1-FEB 2024
For further medical information, please contact:
For UAE ✆ 800 MEDICAL Toll-Free Number.
For all Gulf countries ✆ +971 45 50 38 63 or email: medical-information.gulf@sanofi.com