Pompe Disease
Pompe disease is a rare, progressive, multisystemic, and potentially fatal neuromuscular disorder that predominantly affects cardiac, skeletal, and smooth muscle1,2
-
Pompe disease is an autosomal recessive genetic disorder caused by a deficiency or dysfunction of the lysosomal enzyme acid‑α‑glucosidase (GAA)1
-
GAA deficiency results in lysosomal glycogen accumulation in multiple tissues, with cardiac and skeletal muscle tissues most seriously affected1
-
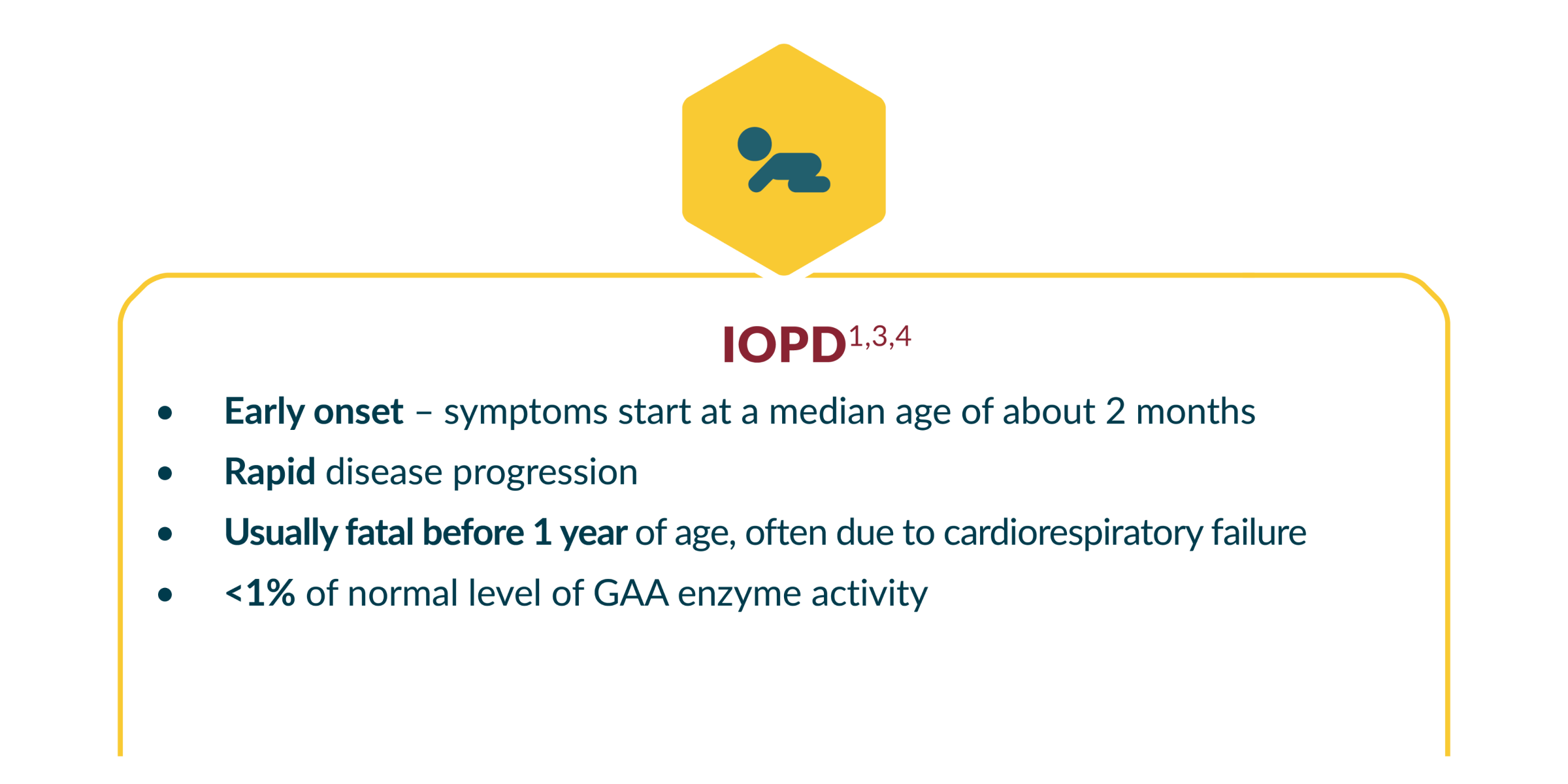
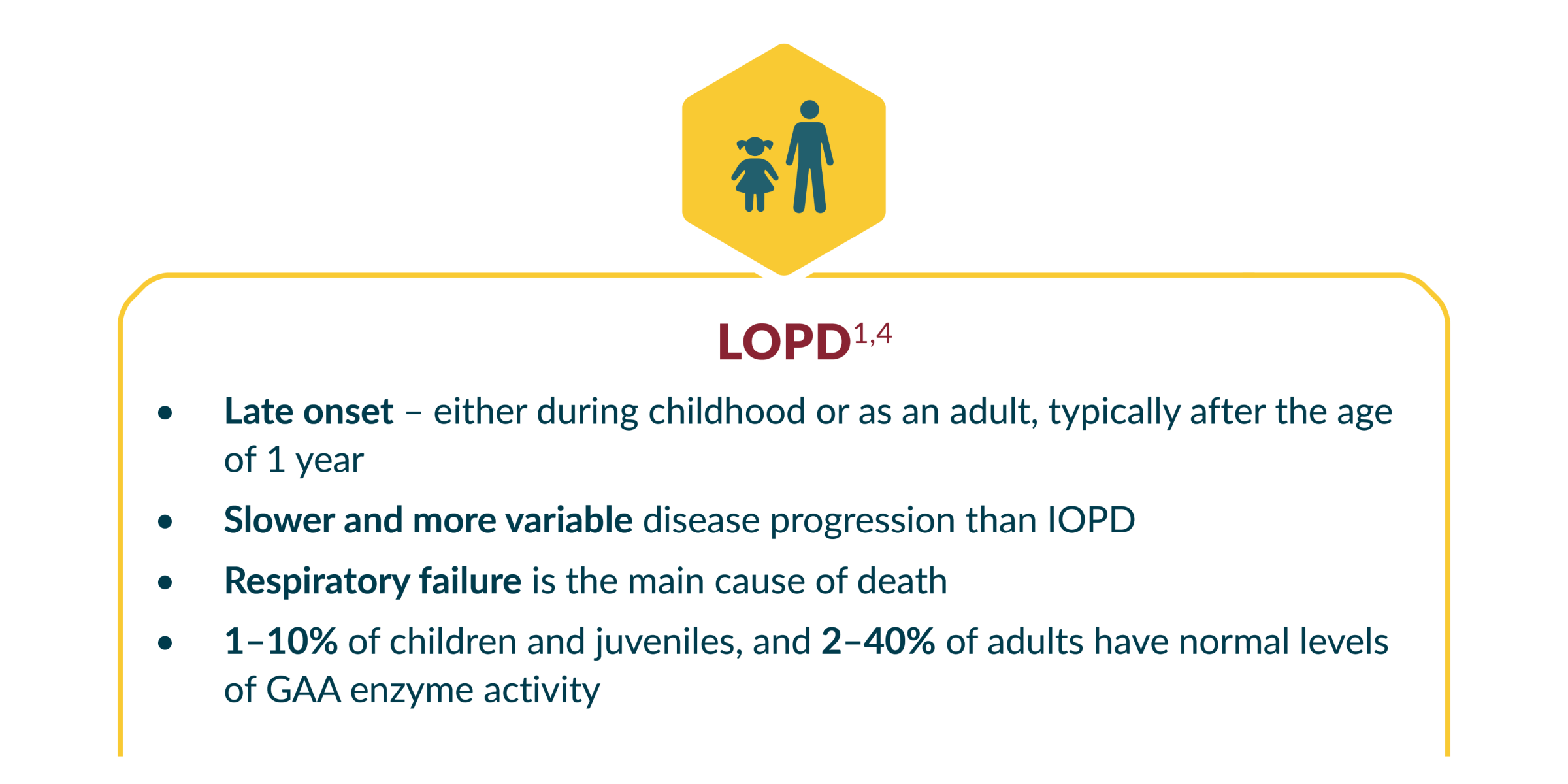
Pompe disease is a single disease continuum with 2 main phenotypes: infantile-onset Pompe disease (IOPD) and late-onset Pompe disease (LOPD)1
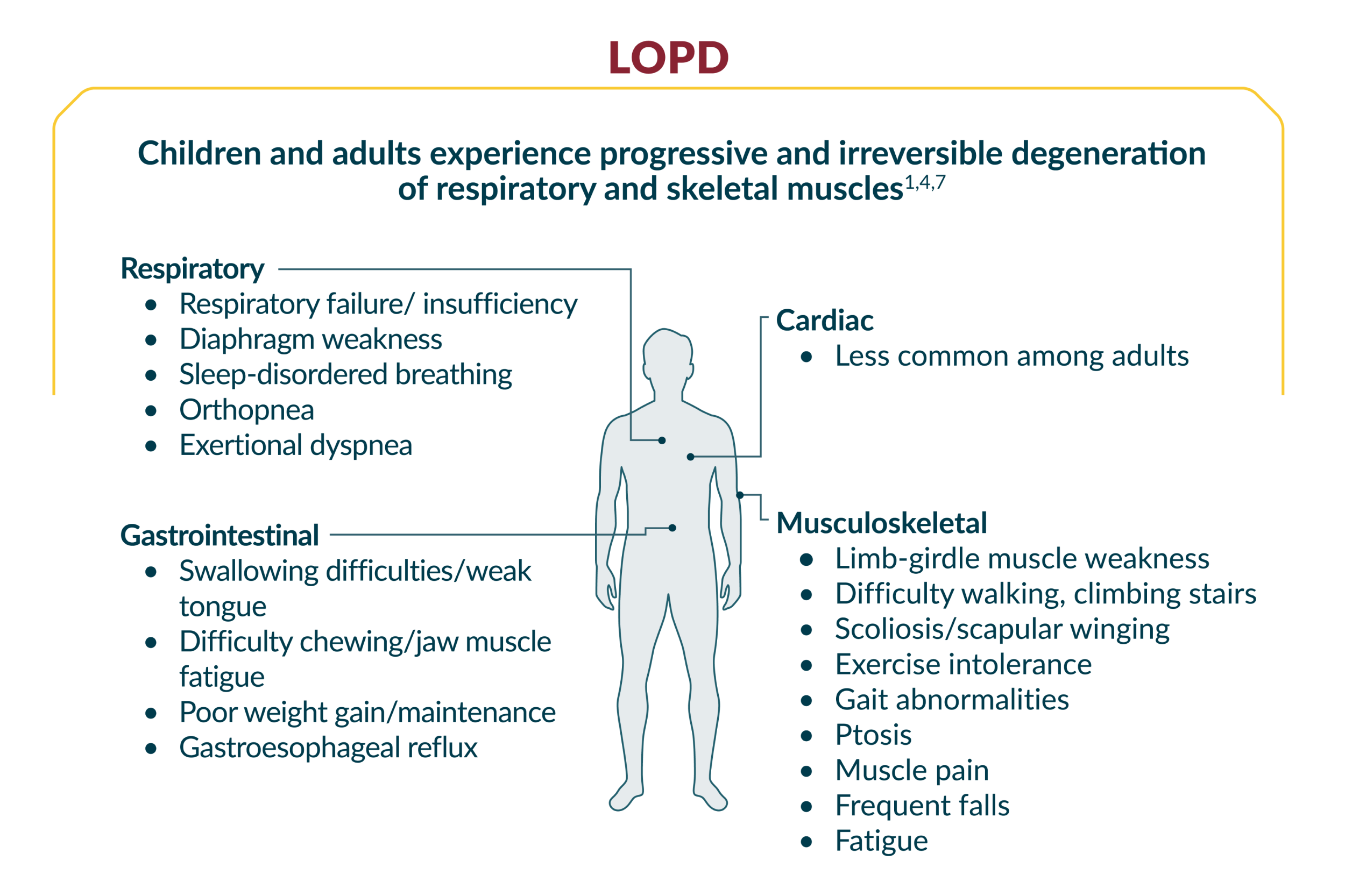
Patients typically present with symptoms that manifest in four organ systems – musculoskeletal, respiratory, cardiac, and gastrointestinal1
What are the symptoms?
Pompe disease affects many parts of the body and can be difficult to diagnose.1,5 Be on the lookout for presenting symptoms and manifestations of Pompe disease.
Symptoms vary between infants with IOPD, and children and adults with LOPD6
In a study of 44 patients (27 females, 17 males) diagnosed with LOPD at the Friedrich-Baur-Institute from 1985–2011:8
77%
of patients with LOPD presented with both exercise intolerance and limb-girdle muscle weakness
55%
of patients with LOPD presented with both respiratory insufficiency (including affected sleep) and limb-girdle muscle weakness
Adapted from Schüller A, et al.
Each year, patients with LOPD are at an increased risk of major disease burdens9,10
In an ongoing research project conducted by the International Pompe Association comprising of 255 patients >2 years of age with LOPD:10
+13%
The chance of needing a wheelchair increased by 13% with every additional year since diagnosis (p<0.001)
+8%
The chance of needing respiratory support increased by 8% with every additional year since diagnosis (p<0.001)
Adapted from Hagemans ML, et al.
If you suspect Pompe disease in one of your patients, take action.
Learn about testing options for Pompe disease
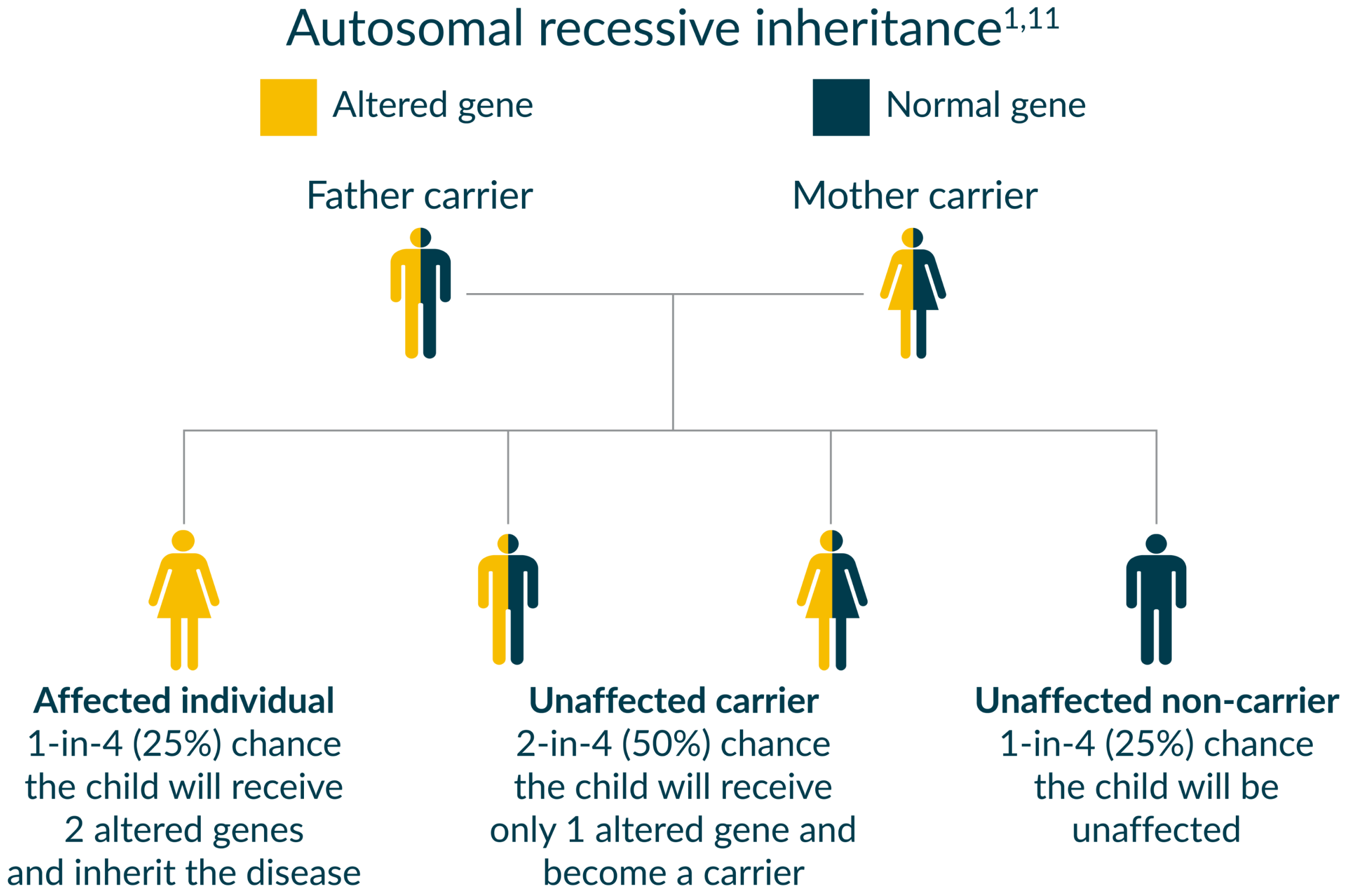
How is Pompe disease inherited?
Have a diagnosed Pompe disease patient? Test their relatives
Early diagnosis is important. DNA mutation analysis of family members can identify additional Pompe disease patients and carriers.1
Sanofi offers GAA enzymatic activity and genetic testing at no cost to physicians and patients suspected of having Pompe disease.
What are some clinical considerations?
Are you looking for Pompe disease?
You play an important role in identifying patients with this progressive, often fatal disease.
![]()
Suspect Pompe disease in patients with these phenotypes:12
Phenotype I: patients presenting with proximal/axial weakness, with or without respiratory symptoms
Phenotype II: patients affected by restrictive respiratory insufficiency
Phenotype III: patients with asymptomatic hyperCKemia*
- In a study of 3,076 adult patients with hyperCKemia and/or limb-girdle muscular weakness (LGMW), gene sequencing found a prevalence of Pompe disease of 2.4%13
- In a study of 275 patients with hyperCKemia and/or limb-girdle phenotype, gene sequencing found a prevalence of Pompe disease of 3.6%14
Would you consider testing for Pompe disease when you see common signs or symptoms?
Download this differential diagnosis checklist for more information
Additional investigations and symptoms:1,12,15
Myopathic EMG pattern
- Signs of spontaneous activity and myotonic discharges
- Often recorded in paraspinal muscles
General physical examination
- Skeletal abnormalities such as scoliosis, lumbar hyperlordosis and rigid spine
Symptoms related to cardiac involvement
- Cardiac arrhythmias, ventricular hypertrophy and Wolf-Parkinson-White syndrome
Symptoms related to respiratory insufficiency
- Dyspnea and obstructive sleep apnea
- History of respiratory infections
- Morning headaches
- Excessive daytime sleepiness
- Weak cough or the decreased effectiveness of cough
Involvement of other organs may include sensorineural hearing impairment, vascular abnormalities with cerebral aneurysms, gastrointestinal involvement with macroglossia, hepatomegaly, diarrhoea and low body mass index.
CK=creatine kinase.
* 1.5 to 15x normal levels; ~300–2000 U/L.
How is Pompe disease diagnosed?
Look for Pompe disease
Diagnosing at an earlier stage of disease allows for earlier treatment intervention and patient management.
-
Symptoms of Pompe disease can resemble those of other diseases, resulting in delayed diagnosis1,5,16
-
The median delay to definitive diagnosis for patients with non-infantile onset Pompe disease can be as much as 7 years5
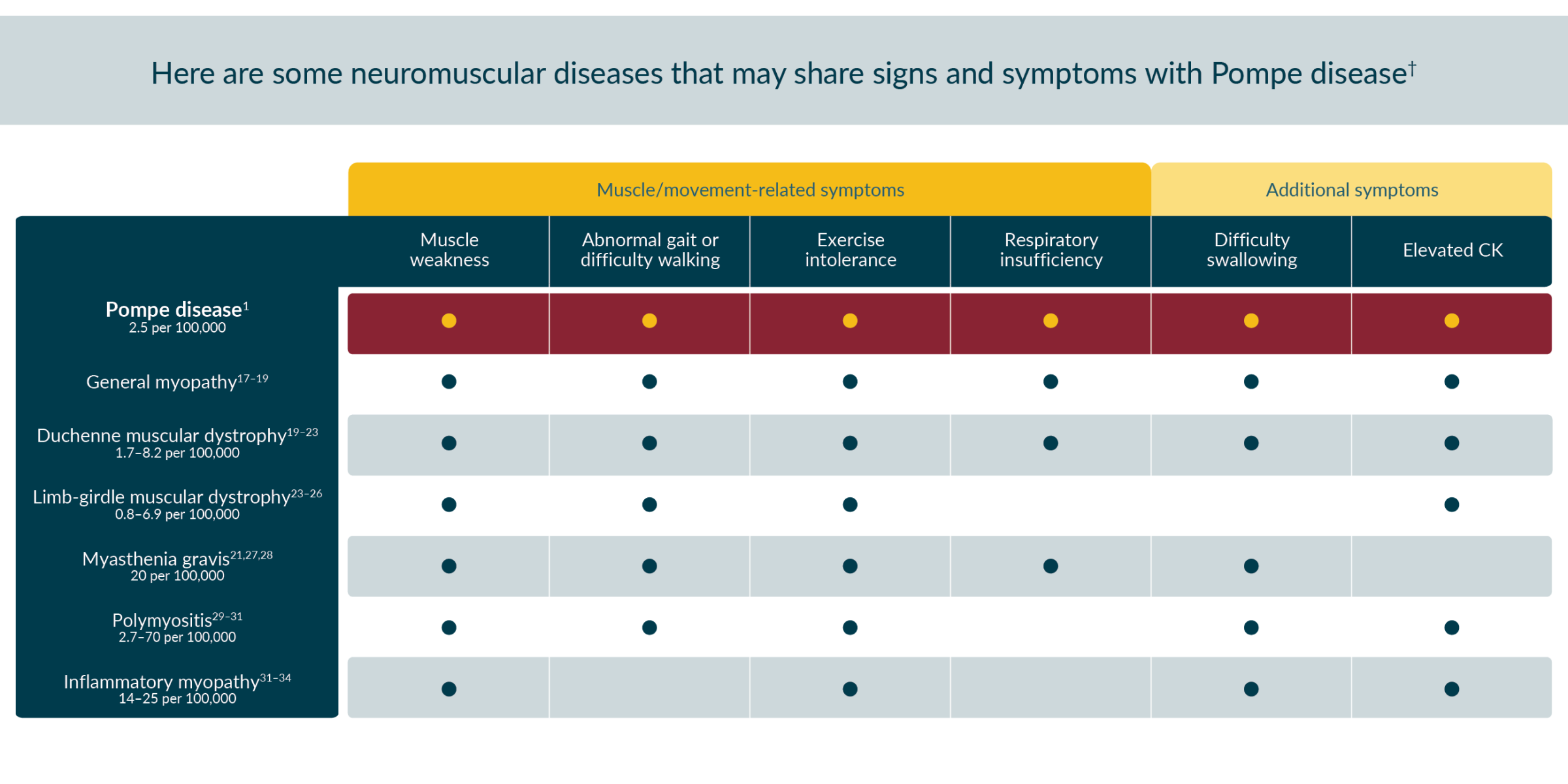
Differential diagnoses in neuromuscular disease
† The signs and symptoms listed in this chart are not an exhaustive list and may not be inclusive of all signs and symptoms that someone with these diseases may encounter.
Testing options for Pompe disease
Testing for enzymatic activity35
This is a relatively quick and non-invasive test that is used when attempting to rule out (or in) Pompe disease specifically. The patient provides a dried blood spot (DBS) sample, which is then tested for the level of activity of the acid α-glucosidase (GAA) enzyme. If enzyme activity is low, the same blood sample can be used for single-gene sequencing of the GAA gene to confirm the Pompe disease diagnosis.
Genetic sequencing36
Genetic sequencing, performed with next-generation sequencing (NGS), supports differential diagnosis by evaluating numerous genetic mutations for symptomatically overlapping disorders simultaneously and rapidly. A muscle disorders genetic panel, like the one offered by Sanofi, can explore over 100 different genetic mutations from one buccal swab patient sample. This type of sequencing can look for known mutations and can also be used to confirm the results of an enzymatic activity test.
Sanofi offers GAA enzymatic activity and genetic testing at no cost to physicians and patients suspected of having Pompe disease.
For more information, please email us here.
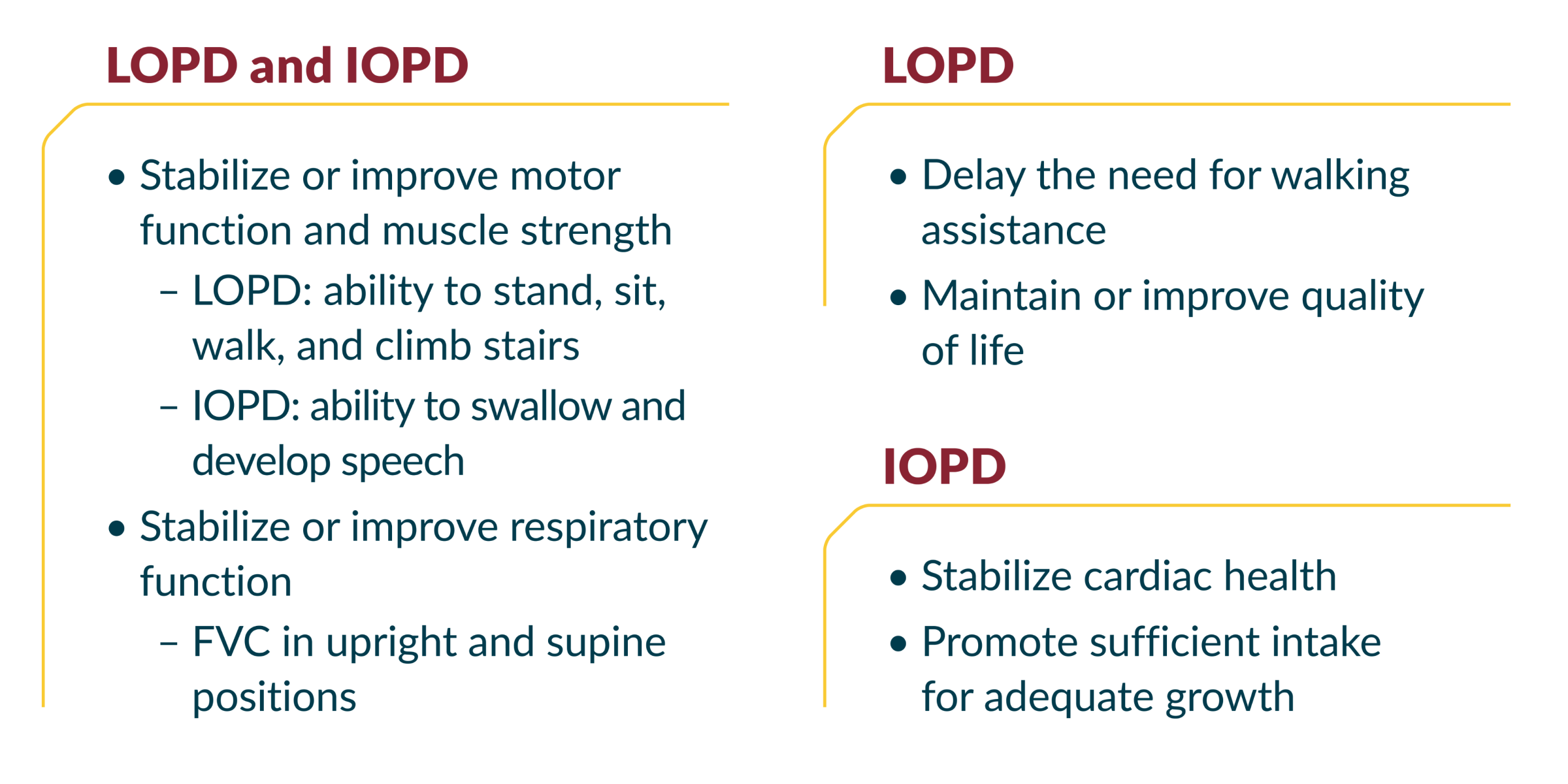
Ongoing management considerations in Pompe disease1,15,37,38
In patients with Pompe disease, early and ongoing multidisciplinary care is key to managing symptoms and improving outcomes1,2,15
Neuromuscular and Pompe Expert Centres
You can also refer your patient to a regional expert centre for the diagnosis, treatment and follow-up of Pompe disease.
Click on your region for the contact information in your province.
Neuromuscular and Pompe Expert Centres in Alberta
CALGARY
Dr. Aneal Khan
Contact: clinic@magiccalgary.ca
Phone: 587-885-3158
Fax: 587-441-8380
Metabolics and Genetics in Calgary (M.A.G.I.C.) Clinic
215–971 64th Ave. NE
Calgary, AB
T2E 7Z4
Dr. Sameer Chhibber
Phone: 587-747-5615
Fax: 587-747-5616
Alberta Neurologic Clinic
Suite 300, 1608 17th Ave. SW
Calgary, AB
T2T 0E3
EDMONTON
Dr. Shailly Jain
Contact: shailly.jain@albertahealthservices.ca
Phone: 780-407-7333
Fax: 780-407-6845
Clinical and Metabolic Genetics Clinic
Department of Medical Genetics
University of Alberta
8–53 Medical Sciences Building
8613 114 Street
Edmonton, AB
T6G 2H7
Dr. Cecile Phan
Contact: phan@ualberta.ca
Phone: 780-248-1698
Fax: 780-407-1507
Kaye Edmonton Neuromuscular Clinic
4C–101, 11400 University Ave. NW
Edmonton, AB
T6G 2G3
Neuromuscular and Pompe Expert Centres in British Columbia
VANCOUVER
Dr. Michelle Mezei
Contact: mezei@mail.ubc.ca
Adult Metabolic Diseases Clinic
2775 Laurel Street
Vancouver, BC
Fax: 604-875-5967
Dr. Anna Lehman
Contact: anna.lehman@vch.ca
Phone: 604-875-5965
Adult Metabolic Diseases Clinic
2775 Laurel Street
Vancouver, BC
Fax: 604-875-5967
Neuromuscular and Pompe Expert Centres in Ontario
HAMILTON
Dr. Mark Tarnopolsky
Phone: 905-521-7933
Fax: 905-521-2638
Department of Medicine
Neuromuscular Disease Clinic
McMaster University H S C 2H22
1200 Main Street
Hamilton, ON
L8N 3Z5
LONDON
Dr. Anita Florendo-Cumbermack
Phone: 519-663-3129
Secretary: Sue Robinson
Fax: 519-663-3328
London Health Sciences Centre
339 Windermere Road
London, ON
N6A 5A5
OTTAWA
Dr. Pierre Bourque
Phone: 613-761-4777
Administrative Assistant: Janine Brooks-Jean
Email: jabrooks@toh.ca
Fax: 613-761-5403
The Ottawa Hospital
1053 Carling Avenue
Ottawa, ON
K1Y 4E9
Neuromuscular and Pompe Expert Centres in Quebec
MONTREAL
Doctors with Pompe experience
Dr. Genge – Neurologist
Dr. O’Ferrall – Neurologist
Dr. Blanchard – Neurologist
Dr. Massie – Neurologist
Contact:
Josée Terrigno
514-398-8551
Institut-Hôpital neurologique de Montréal (MNI – The Neuro)
QUEBEC CITY
Doctors with Pompe experience
Dr. Brunet – Neurologist
Contact:
Manon Gravel – Clinical Nurse
clinique-neuromusculaire@chuquebec.ca
418-525-4444 #66893
Hôpital de l’Enfant-Jésus
SHERBROOKE
Doctors with Pompe experience
Dr. Levesque – Geneticist
Dr. Lareau-Trudel – Neurologist
Contact:
Caroline Barr – Clinical Nurse, Genetics
caroline.barr.ciussse-chus@ssss.gouv.qc.ca
819-346-1110 #16828
Hôpital Fleurimont
- Kishnani PS, et al. Genet Med 2006;8(5):267–88.
- American Association of Neuromuscular & Electrodiagnostic Medicine. Muscle Nerve 2009;40(1):149–160.
- Kishnani PS, et al. J Pediatr 2006;148(5):671–76.
- Kishnani PS, et al. J Pediatr 2004;144:S35–43.
- Winkel LPF, et al. J Neurol 2005;252(8):875–84.
- Hirschhorn R, et al. In: Scriver CR, et al., eds. The Metabolic & Molecular Bases of Inherited Disease. 8th ed. New York, NY: McGraw-Hill; 2001:3389–420.
- Chan J, et al. Molecular Genetics and Metabolism 2017;120(3):163–72.
- Schüller A, et al. In: Am J Med Genet (Part C: Seminars in Medical Genetics) 2012;160(1):80–8. Hoboken: Wiley Subscription Services, Inc.; A Wiley Company.
- Rigter T, et al. Molecular Genetics and Metabolism 2012;107(3):448–55.
- Hagemans ML, et al. Neurology 2005;64(12):2139–41.
- Leslie N, Bailey L. In: Adam MP, et al., eds. GeneReviews 2007 [Updated 2023 Nov 2]. Seattle, WA: University of Washington.
- Toscano A, et al. Acta Myologica 2013;32(2):78.
- Lukacs Z, et al. Neurology 2016;87(3):295–98.
- Savarese M, et al. Neuromuscul Disord 2018;28(7):586–91.
- Tarnopolsky M, et al. Can J Neurol Sci 2016;43(4):472–85.
- Kishnani PS, et al. Am J Med Genet A 2013;161(10):2431–43.
- Barohn RJ, et al. Neurol Clin 2014;32(3):569-vii.
- Hereditary myopathy with early respiratory failure. Genetics Home Reference website. Available at: https://medlineplus.gov/genetics/condition/hereditary-myopathy-with-early-respiratory-failure/. Accessed July 28, 2020.
- Jones K, et al. Interventions for dysphagia in long-term, progressive muscle disease. Cochrane Database Syst Rev 2016 doi: 10.1002/14651858.CD004303.pub4.
- Mah JK, et al. Neuromuscul Disord 2014;24(6):482–91.
- Gilchrist JM. Semin Respir Crit Care Med 2002;23(3):191–200.
- Ozawa E, et al. Mol Cell Biochem 1999;190:143–51.
- Barnabei MS, et al. Compr Physiol 2011;1(3):1353–63.
- Limb-girdle muscular dystrophy. Genetics Home Reference website. Available at: https://medlineplus.gov/genetics/condition/limb-girdle-muscular-dystrophy/#frequency. Accessed July 28, 2020.
- Limb-girdle Muscular Dystrophies NORD website. Available at https://rarediseases.org/rare-diseases/limb-girdle-muscular-dystrophies/. Accessed April 23, 2024.
- Siciliano G, et al. Acta Myol 2015;34(1):3–8.
- Myasthenia gravis. Genetics Home Reference website. Available at: https://medlineplus.gov/genetics/condition/myasthenia-gravis/. Accessed July 29, 2020.
- Myasthenia gravis: what is it? Harvard Health Publishing website. Available at: https://www.health.harvard.edu/a_to_z/myasthenia-gravis-a-to-z. Accessed July 29, 2020.
- Bernatsky S, et al. Ann Rheum Dis 2009;68:1192–96.
- Polymyositis. Johns Hopkins Medicine website. Available at: https://www.hopkinsmedicine.org/health/conditions-and-diseases/polymyositis. Accessed July 29, 2020.
- Mastaglia FL, et al. Rheum Dis Clin North Am 2002;28(4):723–41.
- Smoyer-Tomic KE, et al. BMC Musculoskeletal Disord 2012;13:103.
- Furst D, et al. Muscle & Nerve 2012;45:676–83.
- Inflammatory myopathies information page. National Institute of Neurological Disorders and Stroke website. Available at: https://www.ninds.nih.gov/Disorders/All-Disorders/Inflammatory-Myopathies-Information-Page. Accessed July 29, 2020.
- Taverna S, et al. Aging (Albany NY) 2020;12(15):15856–74.
- Ng KWP, et al. Front Neurol 2022;13:997551.
- Lierena JC Jr, et al. Arq Neuropsiquiatr 2016;74(2):166–76.
- Barba-Romero MA, et al. Rev Neurol 2012;54(8):497–507.
MAT-CA-2301539E - 12/2024





.jpg/jcr:content/image%20(1).jpg)
.jpg/jcr:content/image%20(2).jpg)
.jpg/jcr:content/image%20(3).jpg)