Treatments and challenges for bullous pemphigoid
Systemic corticosteroids and other immunosuppressants are the current mainstay of therapy but carry risks for patients with bullous pemphigoid. Read this article to find out more

A closer look at treating bullous pemphigoid: Unmet needs from a therapeutic management perspective
Traditional management of bullous pemphigoid includes topical and oral corticosteroids1
The European Academy of Dermatology and Venereology (EADV)’s 2022 guidelines for the management of bullous pemphigoid state:*1
- Topical steroids and oral antibiotics can be used to treat mild-to-moderate bullous pemphigoid
- Systemic corticosteroids can be introduced for cases of severe bullous pemphigoid
- For steroid-dependent or recalcitrant bullous pemphigoid, treatment options may include other immunosuppressants (e.g., methotrexate, azathioprine), intravenous immunoglobulins, and B-cell depleting therapy (e.g., rituximab)
These treatment approaches are the current mainstay of therapy and present challenges, particularly in an elderly population with multiple comorbidities and polypharmacy.2–10
*Please refer to local guidelines regarding the regulatory status and approved indications of any medical intervention discussed.
Safety considerations with current treatment options for bullous pemphigoid
Short-term use of topical and medium-dose systemic corticosteroids is considered a safe and e ective first-line approach to managing bullous pemphigoid.1,11 However, the long-term use of systemic corticosteroids (often considered to be greater than 12 months of treatment12) can be associated with severe side e ects, partially due to the advanced age of the patient population1–5
Side effects associated with the long-term use of systemic corticosteroids in bullous pemphigoid
 Steroid- induced myopathy2 |
 Sepsis2,3 |
 Thromboembolic events2 |
 Hypertension4,5 |
 Hyperglycemia/ worsening of diabetes mellitus4,5 |
 Worsening of osteoporosis2,4 ,5 |
 Weight gain4 |
Additionally, the long-term use of other immunosuppressants is associated with an increased risk of adverse events7–9
The long-term safety risks of other immunosuppressive treatments include:
- Hepatotoxicity (methotrexate, azathioprine)7,9
- Nephrotoxicity and hypertension (cyclosporine, methotrexate)8,9
- Thrombophlebitis and thrombosis (mycophenolate mofetil)9
- Gastrointestinal toxicity and distress (azathioprine, mycophenolate mofetil)7
- Increased risk of infection (azathioprine, mycophenolate mofetil)7
- Myelosuppression (azathioprine, methotrexate, cyclosporine)7,9
Due to this potential for adverse events, most of the current immunosuppressive drugs used to treat bullous pemphigoid require frequent lab monitoring1,7
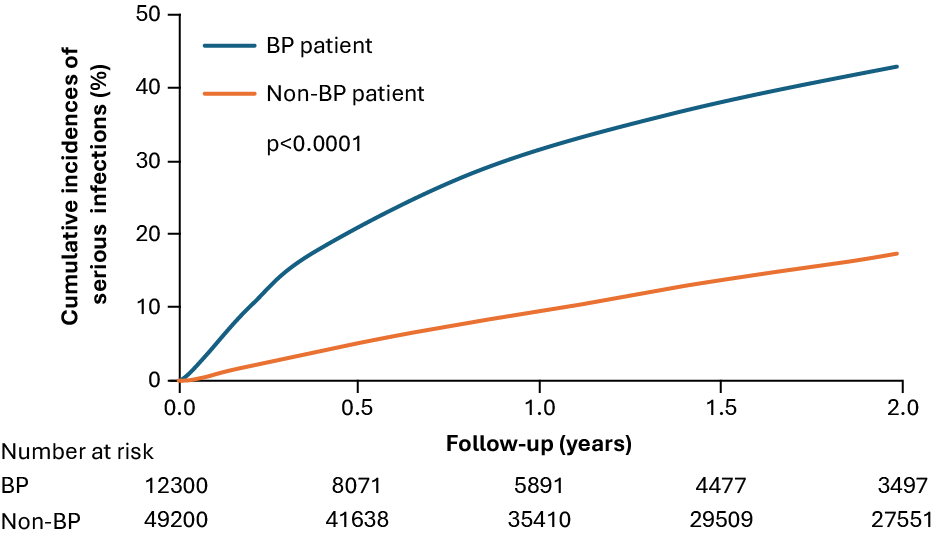
Systemic corticosteroid use is likely a strong predictor of serious infections in patients with bullous pemphigoid3
The use of systemic corticosteroids has been shown to be statistically associated with an increased risk of serious infections in patients with bullous pemphigoid (adjusted hazard ratios: 1.53–2.33, p<0.001). This increased risk of serious infections among systemic corticosteroid users was found to be dose dependent3
The dose-dependent relationship between corticosteroids and serious infection risk highlights the importance of safe and effective therapies in bullous pemphigoid management3
Cumulative incidences of serious infections in bullous pemphigoid (N=5006)3
There is an unmet need in the treatment of bullous pemphigoid
The goals of maintenance therapy for bullous pemphigoid include:13
- Controlling disease activity
- Prompt tapering of systemic corticosteroids (and of adjuvant immunosuppressive agents if applicable) where possible
- Avoiding relapses
- Monitoring of treatment-related adverse effects
With the evolving understanding of the pathophysiology of bullous pemphigoid, there is a need for new advanced therapies that are well-tolerated, provide remission/long-term disease control, and improve patients’ quality of life
|
What is bullous pemphigoid?
|
The challenges of managing bullous pemphigoid
|
Morbidity and mortality in bullous pemphigoid
|
What are the contributing factors in bullous pemphigoid?
|
- Borradori L, et al. J Eur Acad Dermatol Venereol. 2022;36(10):1689–704.
- Pratasava V, et al. Medicina (Kaunas). 2021;57(10):1061.
- Chang T-H, et al. Acta Derm Venereol. 2023;103:adv5329.
- Kirtschig G, et al. Cochrane Database Syst Rev. 2010;2010(10):Cd002292.
- Rice JB, et al. Clin Ther. 2017;39(11):2216–29.
- Khalid SN, et al. Ann Med Surg (Lond). 2021;70:102799.
- Han A. J Clin Aesthet Dermatol. 2009;2(5):19–28.
- Howard SC, et al. Oncologist. 2016;21(12)1471–82.
- Meurer M. Clin Dermatol. 2012;30(1):78–83.
- Försti A-K, et al. Acta Derm Venereol. 2016;96(6):758–61.
- Bernard P and Antonicelli F. Am J Clin Dermatol. 2017;18(4):513–28.
- Persson MS, et al. Br J Gen Pract. 2021;71(713):e904–11.
- Schmidt E, et al. J Dtsch Dermatol Ges. 2020;18(5):516–26.



