How to Diagnose Fabry Disease
Clinical trial summary
Fabry disease and the heart: A comprehensive review
AZEVEDO O, CORDEIRO F, GAGO MF, ET AL. INT J MOLECULAR SCIENCES 2021;22:4434
Non-specific gastrointestinal features: Could it be fabry disease?
HILZ MJ, ARBUSTINI E, DAGNA L, ET AL. DIGESTIVE AND LIVER DISEASE 2018;50:429–437
Fabry disease: A disorder of childhood onset1
SCHIFFMANN R, RIES M. PEDIATRIC NEUROLOGY 2016;64:10-20.
Fabry for Nephrologists - Fabry and Renal
Fabry Disease is a genetic condition that may account for a prevalence of 0.7% of unexplained end-stage renal disease (ESRD) cases.1
People with Fabry disease are at risk of developing ESRD between the third and fifth decades of life.2-5 Signs indicative of early, progressing renal damage which include microalbuminuria and proteinuria developing are seen as early as in the second decade of life.4
Fabry disease results from deficient ɑ-galactosidase A (ɑ-Gal A) activity which causes progressive accumulation of globotriaosylceramide (GL-3) in various cells.4,7,8
- A biopsy may demonstrate GL-3 storage in various cell types and signs of injury, including glomerular sclerosis which may be present as early as childhood9
The European Renal Association-European Dialysis and Transplant Association recommends screening for Fabry disease in:
- male patients with chronic kidney disease (CKD) below 50 years of age in whom a reliable renal diagnosis is absent,
- female patients with unexplained CKD, irrespective of age, and other unexplained symptoms potentially associated with Fabry disease 6
Consider Fabry disease in the differential diagnosis of patients with unexplained renal disease or chronic kidney disease (CKD)
FABRAZYME® 1mg/kg EOW reduced GL-3 accumulation to zero in various types of kidney cells at 54 months including podocytes 10
EOW - (Every other week) every 2 weeks
Agalsidase ß therapy reduced GL-3 accumulation to zero at 54 months in various types of kidney cells. For distal convoluted tubule (DCT)/collecting duct cells, baseline scores were obtained at the beginning of the double-blind trial and at month 54 on a 0 to 3 scale. For all other cell types, pretreatment scores were obtained before agalsidase ß treatment as defined in Materials and Methods. Mesangial cells were scored on a scale of 0 to 2, and other cell types were scored on a scale of 0 to 3.10
Study Design: A randomised, 1:1, double-blind, placebo-controlled study was conducted in 58 patients with Fabry disease, Patients were randomised 1;1 to receive either 1 mg/kg of FABRAZYME® EOW or placebo for 5 months (20 weeks). Inclusion severity at baseline ranged from 0 (normal or near normal) to 3 (severe inclusions).10
Open-label extension of the study: All 58 patients enrolled in the open-label extension study of 54 months in which they received biweekly 1.0 mg/kg FABRAZYME® infusions for up to an additional 54 months.10
Long-term agalsidase β therapy decreases GL-3 accumulation in podocytes. (A) Kidney biopsy that was obtained before agalsidase β therapy exhibits darkstaining granules in podocytes. (B) By month 54, fewer GL-3 inclusions are evident from a specimen that was obtained from the same patient.10
Methylene blue/azure II stain. Magnification, x 400.10
Continued improvement in podocyte clearance was seen at month 54. By month 54, 67% of patients demonstrated a one-point reduction in podocyte GL-3 inclusions from baseline. Although podocytes were not completely cleared of GL-3 deposits, serum creatinine levels remained stable in all but one patient.10
Fabry Disease
A Multisystemic Condition11
Should you wish to test for Fabry, kindly use the contact details below for any DBS kit requests, sample collections or diagnostics related queries:
Email: Ansie.Mienie@nwu.ac.za / pliem@nwu.ac.za
Contact Numbers: 018 299 2312 / 018 285 2544
WhatsApp Number: 082 393 8505
- Tanaka M, et al. Identification of Fabry’s disease by the screening of α-galactosidase A activity in male and female hemodialysis patients. Clinical nephrology. 2005 Oct 1;64(4).
- Schiffmann R, et al. Fabry disease: progression of nephropathy, and prevalence of cardiac and cerebrovascular events before enzyme replacement therapy. Nephrology Dialysis Transplantation. 2009 Jul 1;24(7):2102-11.
- Ortiz A, et al, Fabry Registry. Nephropathy in males and females with Fabry disease: cross-sectional description of patients before treatment with enzyme replacement therapy. Nephrology Dialysis Transplantation. 2008 May 1;23(5):1600-7.
- Germain DP. Fabry disease. Orphanet Journal of rare diseases. 2010 Dec;5(1):1-49
- Ramaswami U, et al. Assessment of renal pathology and dysfunction in children with Fabry disease. Clinical Journal of the American Society of Nephrology. 2010 Feb 1;5(2):365-70.
- Terryn W, et al. Fabry nephropathy: indications for screening and guidance for diagnosis and treatment by the European Renal Best Practice. Nephrology dialysis transplantation. 2013 Mar 1;28(3):505- 17.
- Wanner C, et al. Prognostic indicators of renal disease progression in adults with Fabry disease: natural history data from the Fabry Registry. Clinical Journal of the American Society of Nephrology. 2010 Dec 1;5(12):2220-8.
- Tsutsumi O, et al. Early prenatal diagnosis of inborn error of metabolism: a case report of a fetus affected with Fabry’s disease. Asia‐Oceania Journal of Obstetrics and Gynaecology. 1985 Mar;11(1):39-45.
- Tøndel C, et al. Renal biopsy findings in children and adolescents with Fabry disease and minimal albuminuria. American Journal of Kidney Diseases. 2008 May 1;51(5):767-76.
- Germain DP, et al. Sustained, long-term renal stabilization after 54 months of agalsidase ß therapy in patients with Fabry disease. J Am Soc Nephrol 2007;18:1547-1557.
- Yousef Z, et al. Left ventricular hypertrophy in Fabry disease: a practical approach to diagnosis. European heart journal. 2013 Mar 14;34(11):802-8.
Fabry for Cardiologists - Fabry and Heart
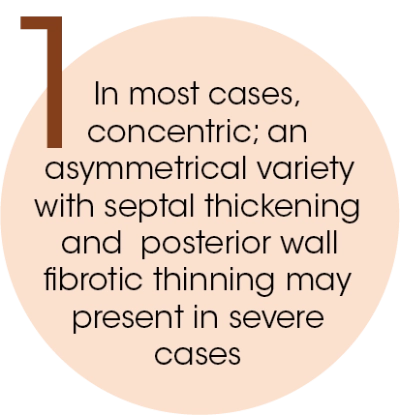
The main manifestation of cardiac involvement in Fabry disease is the progressive thickening of the heart walls expressed as a hypertrophic cardiomyopathy (HCM).1,4
Fabry Disease – A Multisystemic Condition1
Common signs and symptoms of Fabry disease1
In Fabry patients, cardiac involvement may predominate commonly mimicking sarcomeric HCM.2
HCM – Hypertrophic cardiomyopathy
- Registries data suggest that at least 10% of patients may first present with a cardiac event.3
- Cardiac disease is 1 of the 3 major causes of morbidity and mortality in affected males and females.3
The main manifestation of cardiac involvement in Fabry disease is the progressive thickening of the heart walls expressed as a HCM.1,4
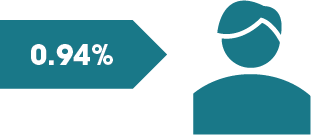
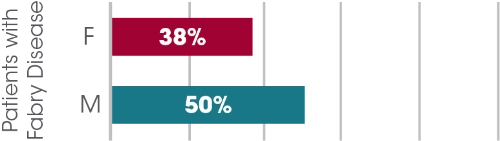
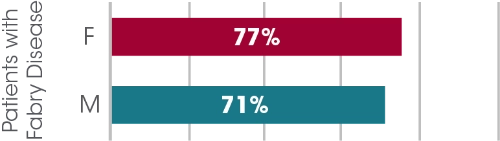
Fabry prevalence in patients with unexplained HCM/LVH5
The intracellular accumulation of Gb3 also occurs within myocytes, valves and vascular endothelium of the heart.4
HCM: Hypertrophic cardiomyopathy; LVH: Left ventricular hypertrophy; Gb3: Globotriaosylceramide
Should you wish to test for Fabry, kindly use the contact details below for any DBS kit requests, sample collections or diagnostics related queries:
Email: Ansie.Mienie@nwu.ac.za / pliem@nwu.ac.za
Contact Numbers: 018 299 2312 / 018 285 2544
WhatsApp Number: 082 393 8505
- Yousef Z, et al. Left ventricular hypertrophy in Fabry disease: a practical approach to diagnosis. European heart journal. 2013 Mar 14;34(11):802-8.
- Brito D, et al . Awareness of Fabry disease in cardiology: A gap to be filled. Revista Portuguesa de Cardiologia (English Edition). 2018 Jun 1;37(6):457-66.
- Fernández A, Politei J. Cardiac manifestation of Fabry disease: from hypertrophic cardiomyopathy to early diagnosis and treatment in patients without left ventricular hypertrophy. Journal of Inborn Errors of Metabolism and Screening. 2019 May 30;4.
- Seydelmann N, et al. Fabry disease and the heart. Best practice & research Clinical endocrinology & metabolism. 2015 Mar 1;29(2):195-204.
- Doheny D, et al. Fabry disease: prevalence of affected males and heterozygotes with pathogenic GLA mutations identified by screening renal, cardiac and stroke clinics, 1995–2017. Journal of medical genetics. 2018 Apr 1;55(4):261-8.
Fabry for Neurologists - Fabry and CNS
The Central Nervous System (CNS) Manifestations and Fabry Disease
include strokes, transient ischaemic attacks (TIAs) and white matter involvement.1,4
Stroke/TIA is often the first serious clinical event in patients with Fabry Disease.2,3
Stroke is a common and serious clinical manifestation of Fabry Disease and can occur in the absence of other key signs of the disease.2
First stroke before diagnosis2
Stroke and Transient Ischaemic Attacks:
Fabry disease puts individuals at increased risk for early TIA and stroke: according to natural history data, 6.9% of males and 4.3% of females experienced strokes with a median age at first stroke being <30 years in males and <45 years in females.3
Progressive accumulation of globotriaosylceramide (GL-3) in the endothelium of intracranial blood vessels is thought to play an important role in the increased risk of ischaemic stroke and TIAs.2
Stroke before any renal or cardiac events2
White Matter Lesions:
A characteristic sign, found in up to 80% of individuals with Fabry disease. These patients show a variable degree of periventricular, deep and/or subcortical white matter involvement. They usually have non-specific distribution and is the most common neuroradiological finding in Fabry Disease.4
The cause of chronic white matter lesions in Fabry disease remains controversial. It is believed that GL-3 related endothelial damage may appear as abnormal hyperintensities in the white matter.3
In patients with Fabry disease, aged 35-45 years, risk of stroke vs the general population is:3
White matter involvement in Fabry disease could range from small, scattered and punctuate T2- weighted hyperintense foci to bilateral diffuse, patchy and partly confluent white matter hyperintensities as seen in the images of a 40-year-old woman (below). Although being the most common neuroimaging finding in Fabry disease, white matter hyperintensities appearance and distribution are not specific in this condition.4
Fabry Disease
A Multisystemic Condition11
Should you wish to test for Fabry, kindly use the contact details below for any DBS kit requests, sample collections or diagnostics related queries:
Email: Ansie.Mienie@nwu.ac.za / pliem@nwu.ac.za
Contact Numbers: 018 299 2312 / 018 285 2544
WhatsApp Number: 082 393 8505
- Ortiz A, et al. Fabry disease revisited: Management and treatment recommendations for adult patients. Molecular genetics and metabolism. 2018 Apr 1;123(4):416-27.
- Sims K, et al. Stroke in Fabry disease frequently occurs before diagnosis and in the absence of other clinical events: natural history data from the Fabry Registry. Stroke. 2009 Mar 1;40(3):788-94.
- Kolodny E, et al. Cerebrovascular involvement in Fabry disease: current status of knowledge. Stroke. 2015 Jan;46(1):302-13.
- Cocozza SA, et al. Neuroimaging in Fabry disease: current knowledge and future directions. Insights into imaging. 2018 Dec;9(6):1077-88.
- Yousef Z, et al. Left ventricular hypertrophy in Fabry disease: a practical approach to diagnosis. European heart journal. 2013 Mar 14;34(11):802-8.
Fabry for Neurologists and Physicians
Peripheral Nervous System manifestations include pain and auditory abnormalities.1
Extremity pain is one of the earliest and most common clinical symptoms of Fabry disease.2,3
It typically manifests as episodes of burning, stabbing, tingling or shooting pain and has a significant impact on a patient’s quality of life.2,3
Pain:
Pain in Fabry disease is multimodal, driven by multiple diverse pathophysiological mechanisms.2
Globotriaosylceramide (GL-3) accumulation in the dorsal root ganglia and microvascular endothelium results in small fiber neuropathy, ischaemia and axonal degeneration.1,2
Pain may also be due to ectopic discharges, altered pain modulation and central nervous system sensitisation.1,2
- One of the earliest and most common clinical symptoms of Fabry disease.2
- Typically manifests as episodes of burning, stabbing, tingling or shooting pain.2
- Begins in the distal extremities and radiates proximally.2
- May manifest as ‘pain crises’, which are attacks of excruciating pain that may spread over the entire body.2
- Most important triggers of pain are physical exercise, thermal stimuli, and fever.2
- Has a significant physical and social impact on a patient’s quality of life and may contribute to depression, anxiety and illicit drug use to manage the pain.2,3
Auditory and vestibular abnormalities:
Hearing loss, tinnitus and vertigo occurs in Fabry disease, potentially due to narrowing of cochlear and vestibular vessels, globotriaosylceramide (GL-3) deposition in spiral ganglia and vestibular structures and ischaemic auditory neuropathy.1
- Frequently observed symptoms which include hearing loss, tinnitus and vertigo.1
- High incidence of both progressive hearing Loss and sudden deafness has been demonstrated in males with classic Fabry disease.
- Pain
- Auditory abnormalities
- Headaches
- Depression
- Fatigue
- Stroke
- Transient ischaemic attacks
- White matter lesions
- Abnormalities of intercranial vessels
- Premature death
Fabry Disease
A Multisystemic Condition11
Should you wish to test for Fabry, kindly use the contact details below for any DBS kit requests, sample collections or diagnostics related queries:
Email: Ansie.Mienie@nwu.ac.za / pliem@nwu.ac.za
Contact Numbers: 018 299 2312 / 018 285 2544
WhatsApp Number: 082 393 8505
- Ortiz A, et al. Fabry disease revisited: management and treatment recommendations for adult patients. Molecular genetics and metabolism. 2018 Apr 1;123(4):416-27.
- Politei JM, et al. Pain in Fabry disease: practical recommendations for diagnosis and treatment. CNS Neuroscience & Therapeutics. 2016 Jul;22(7):568-76.
- Germain DP. Fabry disease. Orphanet Journal of rare diseases. 2010 Dec;5(1):1-49.
- Sims K, et al . Stroke in Fabry disease frequently occurs before diagnosis and in the absence of other clinical events: natural history data from the Fabry Registry. Stroke. 2009 Mar 1;40(3):788-94.
- Burlina AP, et al. Early diagnosis of peripheral nervous system involvement in Fabry disease and treatment of neuropathic pain: the report of an expert panel. BMC Neurology. 2011 Dec;11(1):1-11.
- Yousef Z, et al. Left ventricular hypertrophy in Fabry disease: a practical approach to diagnosis. European heart journal. 2013 Mar 14;34(11):802-8.



.webp)
.webp)
.webp)