How to Diagnose Gaucher Disease
Clinical trial summary
Finding and treating Gaucher Disease Type 1 The role of the haematologist
CAPPELLINI M-D, CASSINERIO E, MOTTA I, ET AL. EUR ONCOL & HAEMATOL 2018;14(1):50-56.
Gaucher Disease in Adults
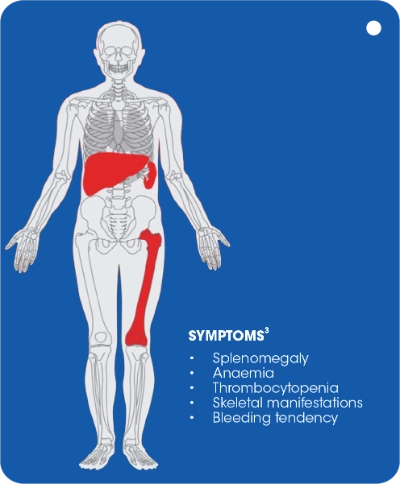
- The early signs and symptoms of Gaucher disease Type 1 tend to reflect the haematological aspects of the disease (splenomegaly, anaemia, thrombocytopenia and bleeding tendency), but skeletal manifestations are often present2
- Splenomegaly and/or thrombocytopenia are the 2 most prominent and frequent-presenting symptoms of Gaucher disease2,19
- Skeletal manifestations are prevalent at all ages and are the principal cause of pain, disability and reduced quality of life20
- Gaucher disease affects the Bone Mineral (BM) and the mineralised components of bone. Changes include BM infiltration and plasma cell dyscrasias; modelling and remodelling abnormalities of bones, resulting in developmental changes and loss of bone mineral (osteopenia/osteoporosis), cortical thinning, lytic lesions and fragility fractures; and osteonecrosis and related phenomena (medullary infarctions, osteosclerosis, cortical infarcts and joint destruction and deformities)20
Diagnostic algorithm for adults of non-ashkenazi jewish descent
MGUS = Monoclonal Gammopathy of Undermined Significance.
Adapted from Mistry PK et al. Am J Hematol. 2011;86(1):110-115.
- Gaucher disease is an autosomal recessive disorder caused by deficient activity of the lysosomal enzyme acid-ß-glucosidase (glucocerebrosidase, or glucosylceramidase, or GBA1), resulting in progressive accumulation of glucosylceramide mainly in macrophages. These lipid-laden macrophages (also called Gaucher cells) start accumulating in the bone marrow and spleen, leading to a spectrum of debilitating visceral, haematologic and skeletal manifestations2,3.
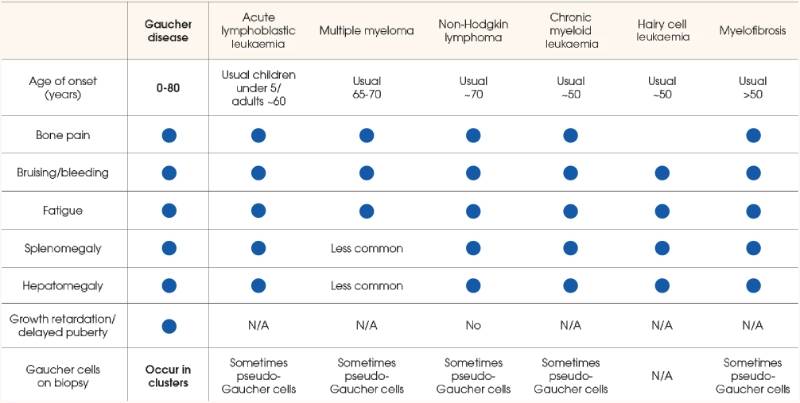
Gaucher disease most commonly mimics the signs and symptoms of many haematological malignancies4-18.
Consider gaucher disease in your differential diagnosis once malignancy has been ruled out1.
Should you wish to test a patient for GAUCHER DISEASE, kindly refer them to your local lab for a DBS (Dried Blood Spot) test. For any DBS sample collections, kit requests, or diagnostic related queries, kindly contact:
Email: pliem@nwu.ac.za/Ansie.Mienie@nwu.ac.za
Contact number: 018 299 2312/018 285 2544
WhatsApp number: 082 393 8505
- Cappellini M-D, Cassinerio E, Motta I, et al. Finding and treating Gaucher disease Type 1. The role of the haematologist. Eur Oncol & Haematol. 2018;14(1):50-56.
- Mistry PK, Cappellini MD, Lukina E, et al. A reappraisal of Gaucher disease - diagnosis and disease management algorithms. Am J Hematol. 2011;86(1):110-115.
- Mistry PK, Sadan S, Yang R, et al. Consequences of diagnostic delays in Type 1 Gaucher disease: the need for greater awareness among haematologist-oncologists and an opportunity for early diagnosis and intervention. Am J Hematol. 2007;82(8):697-70.
- Grabowski GA, Petsko GA, Kolodny EH. Chapter 146: Gaucher disease. Valle D, Beaudet AL, Vogelstein B, et al, eds. The Online Metabolic and Molecular Bases of Inherited Disease. New York, NY: McGraw Hill; 2014. http://ommbid.mhmedical.com/content. aspx?bookid=474§ionid=45374148. Accessed July 14, 2014.
- Haematology: basic principles and practice, 6th edition. Hoffman R, Benz EJ, Silberstein LE, Heslop HE, Weitz JI, Anastasi J, eds. Philadelphia, PA: Saunders, an imprint of Elsevier Inc.; 2013.
- O’Donnell M. Acute leukaemias. Cancer management. Cancer network website. http:// www.cancernetwork.com/cancer-management/acute-leukemias. Accessed December 1, 2014.
- Shankland KR, Armitage JO, Hancock BW. Non-hodgkin lymphoma. The Lancet. 2012 Sep 1;380(9844):848-57.
- Al-Farsi K. Multiple myeloma: an update. Oman Med J. 2013; 28(1)3-11.
- Shah D. Multiple myeloma clinical presentation. Medscape website. http://emedicine.medscape.com/article/204369-clinical. Accessed December 1, 2014.
- Adult non-Hodgkin lymphoma treatment (PDQ(R)). National Cancer Institute website. http://cancer.gov/cancertopics/pdq/treatment/adult-non-hodgkins/Patient. Updated April 25, 2014. Accessed December 1, 2014.
- Savage DG, Szydlo RM, Goldman JM. Clinical features at diagnosis in 430 patients with chronic myeloid leukaemia seen at a referral centre over a 16-year period. Br J Haematol. 1997;96(1): 111-116.
- Sawyers CL. Chronic myeloid leukaemia. N Engl J Med. 1999;340(17):1330-1340.
- Faderl S, Talpaz M, Estrov Z, et al. The biology of chronic myeloid leukaemia. N Engl J Med. 1999;341(3):164-172.
- Hairy cell leukaemia treatment (PDQ(R)). National Cancer Institute website. http://cancer.gov/cancertopics/pdq/treatment/hairy-cell-leukaemia/Patient. Updated November 11, 2014. Accessed December 1, 2014.
- Hairy cell leukaemia facts (FS16). Leukaemia & Lymphoma Society. White Plains, NY; October 2013.13. Myelofibrosis facts (FS14). Leukaemia & Lymphoma Society. White Plains, NY; October 2013.
- Myelofibrosis facts (FS14). Leukaemia & Lymphoma Society. White Plains, NY; October 2013.
- Tefferi A. Primary myelofibrosis: 2013 update on diagnosis, risk-stratification and management. Am J Hematol. 2013;88(2):141-150.
- Thiele J, Kvasnicka HM, Schmitt-Graeff A, et al. Effects of the tyrosine kinase inhibitor imatinib mesylate (STI571) on bone marrow features in patients with chronic myelogenous leukaemia. Histol Histopathol. 2004;19(4):1277-1288.
- Gaucher registry annual report. Genzyme Corp. 2006.
- Hughes D, Mikosch P, Belmatoug N, Carubbi F, Cox T, Goker-Alpan O, Kindmark A, Mistry P, Poll L, Weinreb N, Deegan P. Gaucher disease in bone: from pathophysiology to practice. Journal of Bone and Mineral Research. 2019 Jun;34(6):996-1013.
Gaucher Disease in Children
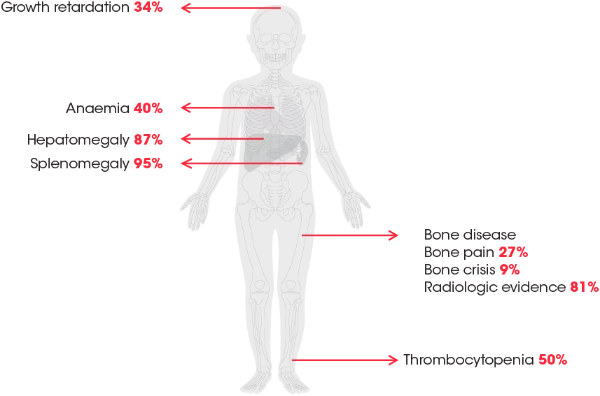
Children have a high incidence of organ involvement1
► Splenomegaly is the most prominent and frequent-presenting symptom of Gaucher disease¹
Adapted from Kaplan P, et al. Arch Pediatr Adolesc Med. 2006;160(6):603-608.
Gaucher Disease
Gaucher disease is an Autosomal recessive disorder1,4
- Deficient activity of the lysosomal enzyme acid ß-glucosidase (GBA1) leads to the progressive storage of glucosylceramide in macrophages and other cells1,5,6
- Accumulation of lipid-laden “Gaucher cells” causes a spectrum of debilitating visceral, haematologic and skeletal manifestations6
Gaucher disease with onset in childhood is typically more severe and rapidly progressive1,5
- It is associated with1:
- Substantial morbidity
- Potential for disability
- Reduced life expectancy
- Untreated children may be at high risk for irreversible complications1
- It may greatly impact quality of life1:
- Delayed puberty may affect body image and social functioning in older children3,5
- Increased awareness of ‘‘being different’’ may be amplified when symptoms prevent children from participating in sports and other activities5
Consider Gaucher disease in children with splenomegaly, with or without hepatomegaly, thrombocytopenia and/or anaemia when a detailed medical history, physical exam and laboratory tests are not suggestive of malignancy1
- Gaucher disease in children mimics the signs and symptoms of haematological malignancies1,2,5,7-15.
- The early signs and symptoms of Gaucher disease in children tend to reflect the visceral and haematological aspects of the disease1,2,6.
- Gaucher disease should be considered when a detailed medical history, physical exam and laboratory tests are not suggestive of malignancy2.
Consider gaucher disease in your differential diagnosis.
Should you wish to test a patient for GAUCHER DISEASE, kindly refer them to your local lab for a DBS (Dried Blood Spot) test. For any DBS sample collections, kit requests, or diagnostic related queries, kindly contact:
Email: pliem@nwu.ac.za/Ansie.Mienie@nwu.ac.za
Contact number: 018 299 2312/018 285 2544
WhatsApp number: 082 393 8505
- Kaplan P, Andersson HC, Kacena KA, Yee JD. The clinical and demographic characteristics of non-neuronopathic Gaucher disease in 887 children at diagnosis. Arch Pediatr Adolesc Med. 2006;160(6):603-608.
- Di Rocco M, Andria G, Deodato F, Giona F, Micalizzi C, Pession A. Early diagnosis of Gaucher disease in pediatric patients: proposal for a diagnostic algorithm. Pediatr Blood Cancer. 2014;61(11):1905-1909.
- Kaplan P, Baris H, De Meirleir L, et al. Revised recommendations for the management of Gaucher disease in children. Eur J Pediatr. 2013;172(4):447-458.
- Mistry PK, Sadan S, Yang R, Yee J, Yang M. Consequences of diagnostic delays in type 1 Gaucher disease: the need for greater awareness among hematologists-oncologists and an opportunity for early diagnosis and intervention. Am J Hematol. 2007;82(8):697-701.
- Grabowski GA, Andria G, Baldellou A, et al. Pediatric non-neuronopathic Gaucher disease: presentation, diagnosis and assessment. Consensus statements. Eur J Pediatr. 2004;163(2):58-66.
- Mistry PK, Cappellini MD, Lukina E, et al. A reappraisal of Gaucher disease-diagnosis and disease management algorithms. Am J Hematol. 2011;86(1):110-115.
- Chen M, Wang J. Gaucher disease. Review of the literature. Arch Pathol Lab Med. 2008;132(5):851-853.
- Hoffman R, Benz EJ, Silberstein LE, Heslop H, Weitz J, Anastasi J, eds. Hematology: Basic Principles and Practice. 6th ed. Philadelphia, PA: Saunders, an imprint of Elsevier Inc.; 2013.
- Shankland KR, Armitage JO, Hancock BW. Non-Hodgkin lymphoma. Lancet. 2012;380(9844):848-857.
- West SG. Systemic disease in which arthritis is a feature. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 24th ed. Philadelphia, PA: Elsevier, Inc.; 2012.
- Sawyers CL. Chronic myeloid leukemia. N Engl J Med. 1999;340(17):1330-1340.
- Savage DG, Szydlo RM, Goldman JM. Clinical features at diagnosis in 430 patients with chronic myeloid leukaemia seen at a referral centre over a 16-year period. Br J Haematol. 1997;96(1):111-116.
- Tefferi A. Primary myelofibrosis: 2013 update on diagnosis, risk-stratification, and management. Am J Hematol. 2013;88(2):141-150.
- Grabowski GA, Petsko GA, Kolodny EH. Chapter 146: Gaucher disease. Valle D, Beaudet AL, Vogelstein B , et al, eds. The Online Metabolic and Molecular Bases of Inherited Disease. New York, NY: McGraw Hill; 2014.
- Thiele J, Kvasnicka HM, Schmitt-Graeff A, et al. Effects of the tyrosine kinase inhibitor imatinib mesylate (STI571) on bone marrow features in patients with chronic myelogenous leukemia. Histol Histopathol. 2004;19(4):1277-1288.


.jpg)

.jpg)
.webp)
.webp)