146 for Lipid Management After ACS
ACS patients at very high risk – remember 146*1
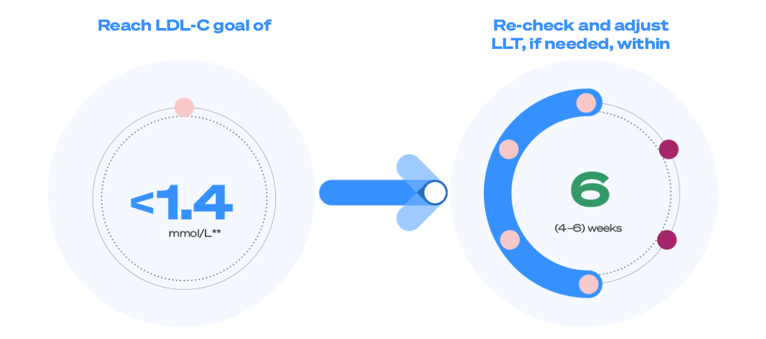
The 2019 ESC/EAS dyslipidaemia guidelines recommend that post-ACS patient achieve an LDL-C value of less than 1.4 mmol/L.
Lipids levels should be reassessed 4-6 weeks after an ACS event, and if the target is not met, lipid-lowering treatments should be adjusted accordingly.
Did you know there is a very simple way to remember this for patients at very high CV risk?1†
In the video below, you can hear Prof. A. Catapano explain the concept in 1 minute
To reach the <1.4 mmol/L LDL-C goal the ACVC/EAPC/ESC propose a strike early and strong approach to post-ACS LDL-C lowering:1,2‡
- Initiate combination LLT with a statin + ezetimibe as soon as possible post-ACS
- Consider the addition of a PCSK9i in the acute phase, particularly in ACS patients with high-risk features.
Following the latest guidelines, for your patients at very high CV risk, remember 146.1*
*According to the ESC/EAS dyslipidaemia guidelines, after an ACS, patients are recommended to reach anLDL-C value of <55 mg/dL (<1.4 mmol/L). Lipid levels should be re-evaluated 4–6 weeks after an ACS. If the treatment goal has not been reached, lipid-lowering treatment should be adjusted. Within ”146”, ”14” reflects the <1.4 mmol/L recommended goal for patients after ACS and “6” reflects the maximum time recommended to re-evaluate LDL-C levels.1
†ESC/EAS dyslipidaemia guidelines recommend an LDL-C reduction of ≥50% from baseline and an LDL-C goal of <1.4 mmol/L for secondary prevention in patients at very high CV risk (Class I, Level A). Lipid levels should be re-evaluated 4–6 weeks after ACS to determine whether treatment goals have been achieved and to check for any safety issues; the therapeutic regimen can then be adapted accordingly. If the LDL-C goal is not achieved after 4–6 weeks despite maximal tolerated statin therapy and ezetimibe, addition of a PCSK9i is recommended.1
‡Based on clinical trial and observational study evidence supporting early and strong LDL-C reduction, the ACVC in collaboration with the EAPC and ESC proposed the following lipid-lowering algorithm in a clinical consensus statement: combination therapy consisting of a high-intensity statin and ezetimibe, preferably as a combination pill, should be initiated as soon as possible, preferably before coronary angiography, irrespective of LDL-C levels or pre-existing statin therapy. A lipid panel should be obtained as early as possible. Treatment with a PCSK9i in the acute phase may be discussed, especially in patients exhibiting additional high-risk features such as multivessel coronary disease, polyvascular disease or FH. In patients experiencing a second major vascular event while treated with a high-intensity statin, current ESC dyslipidaemia guidelines suggest an LDL-C goal of <1.03 mmol/L for which a PCSK9i would be necessary in most patients. All patients, particularly those with very high untreated LDL-C of >4.91 or >4.14 mmol/L in the presence of premature AMI or family history of premature AMI, should be screened for FH. All patients should be discharged with a clear lipid improvement plan and be re-evaluated after 4–6 weeks in a specialised secondary prevention clinic and achieved LDL-C, treatment tolerability, compliance and knowledge about disease and therapies should be assessed. Lipid-lowering therapy should be escalated if goals are not met. In patients with known statin intolerance, statin treatment should be re-initiated at the maximally tolerated dose in combination with ezetimibe and a PCSK9i. If a PCSK9i is not available, bempedoic acid may represent an alternative. In case of a recurrence of symptoms suggestive of recurrent statin intolerance, re-challenge with an alternative statin should be attempted. In patients prescribed a PCSK9i in the acute phase for fast LDL-C goal achievement and/or stabilisation of the remaining coronary vasculature, de-escalation of triple therapy (high-intensity statin, ezetimibe and PCSK9i) should be discussed during follow-up.2
ACS = acute coronary syndrome; ACVC = Association for Acute Cardiovascular Care; AMI = acute myocardial infarction; CV = cardiovascular; EAPC = European Association of Preventive Cardiology; EAS = European Atherosclerosis Society; ESC = European Society of Cardiology; FH = familial hypercholesterolaemia; LDL-C = low-density lipoprotein cholesterol; LLT = lipid-lowering therapy; PCSK9i = proprotein convertase subtilisin kexin type 9 inhibitor.
Referanser
-
Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111–188.
-
Krychtiuk KA, Ahrens I, Drexel H, et al. Acute LDL-C reduction post ACS: strike early and strike strong: from evidence to clinical practice. A clinical consensus statement of the Association for Acute Cardiovascular Care (ACVC), in collaboration with the European Association of Preventive Cardiology (EAPC) and the European Society of Cardiology Working Group on Cardiovascular Pharmacotherapy. Eur Heart J Acute Cardiovasc Care. 2022;11(12):939–949.