Clinical presentation and pathophysiology of Prurigo Nodularis (PN)
Explore the clinical presentation and pathophysiology of Prurigo Nodularis (PN), including its systemic inflammation, itching-scratching cycle, and effects on quality of life. Learn about the underlying mechanisms and treatment options for this chronic skin condition.
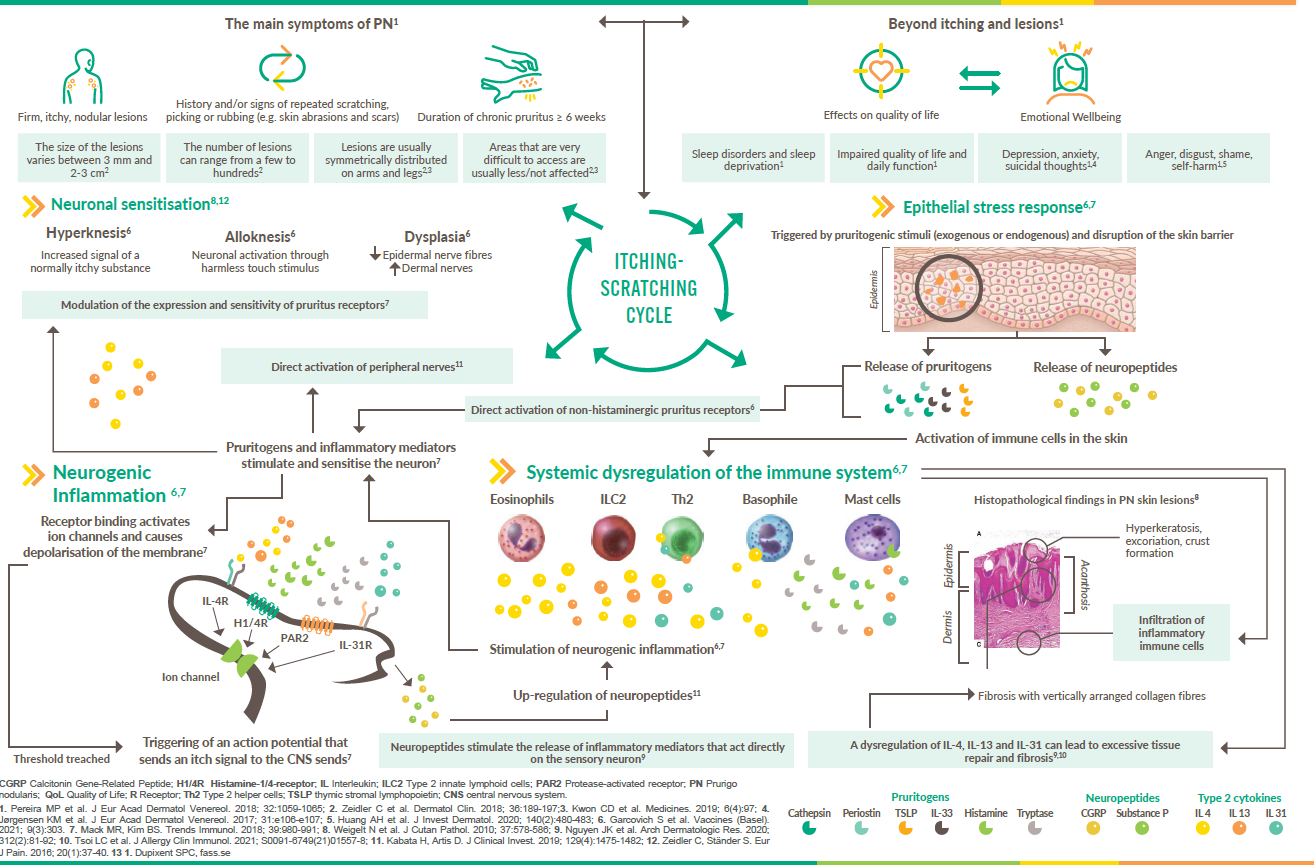
Although the exact pathogenesis of Prurigo nodularis (PN) is not yet fully understood, it is an independent disease entity with an underlying systemic inflammation.1,2
PN is a disease with severe itching characterised by impaired signalling between the skin, the nervous system and the immune system.2 Epidermal stress and inflammatory responses of the skin to pruritus lead to activation of immune cells and release of type 2 cytokines and other inflammatory mediators.2,3 The inflammatory mediators released by the dermal infiltrate directly activate receptors on sensory neurones and/or modulate the expression and sensitivity of pruritus receptors.2,3 This leads to the release of neuropeptides that stimulate and enhance neuronal function, resulting in nerve dysplasia and neuronal hypersensitivity.2,3 This neuronal transmission to the central nervous system and nearby efferent neurons triggers itching and promotes the itch-scratch cycle, which in turn favours neurogenic and cutaneous inflammation, barrier defects, skin remodelling and the development of lesions.2,3

Pruritus can be multifactorial and become chronically persistent. PN is characterised by a disturbed interaction between the nerve cells, the immune system and the skin.1
-
Elmariah S et al. J Am Acad Dermatol. 2021; 84(3):747-776;
-
Garcovich S, et al. Vaccines (Basel). 2021; 9(3):303;
-
Mack MR, Kim BS. Trends Immunol. 2018; 39(12):980-991.