Pompe disease
What is Pompe disease?
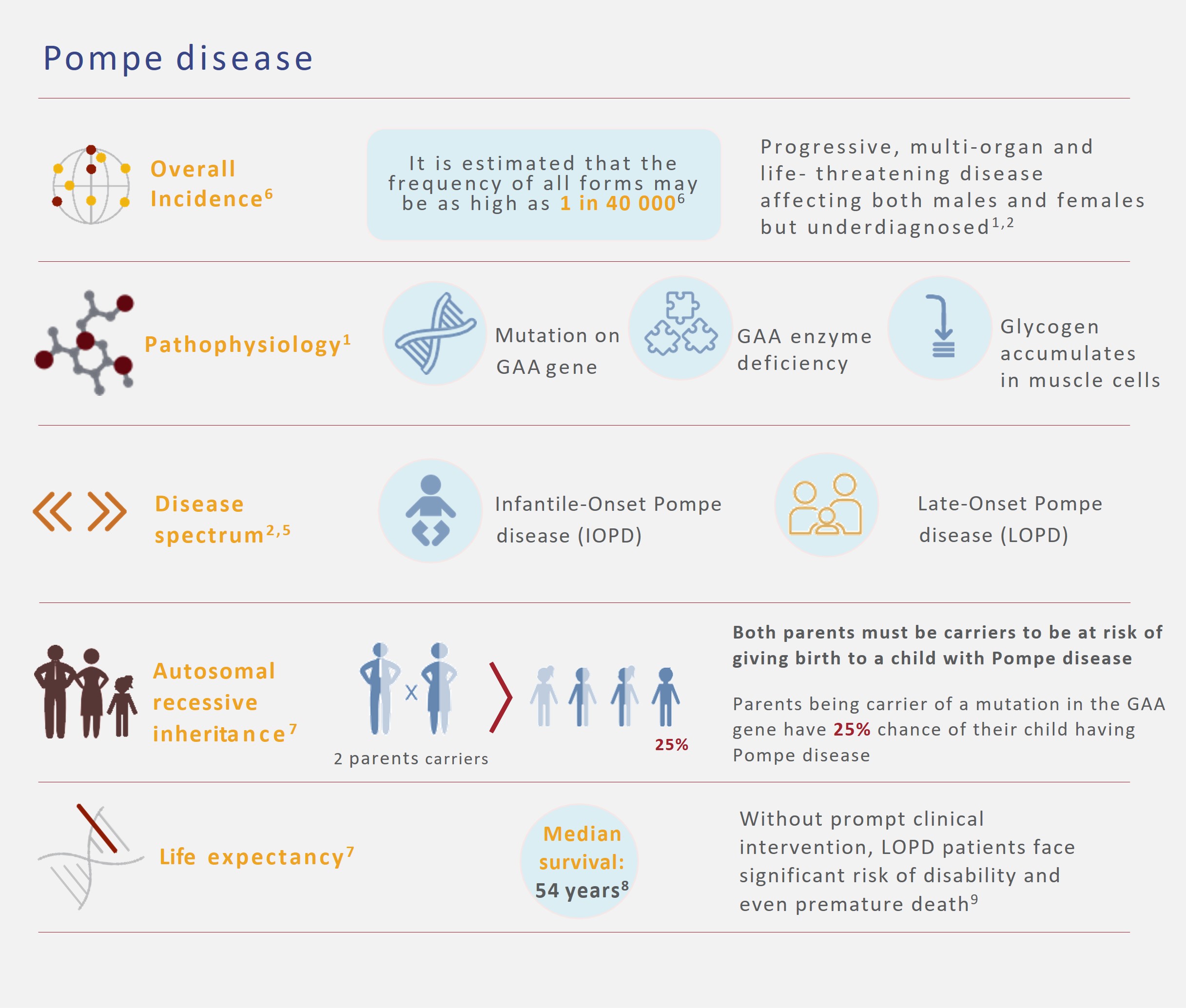
Pompe disease is an autosomal recessive lysosomal storage disorder caused by mutations in the gene encoding acid a-glucosidase (GAA) or acid maltase. The accumulation of its substrate, glycogen, is associated with a broad spectrum of clinical symptoms and varying degrees of progression, symptom onset, organic impairment and severity. Glycogen buildup occurs in various tissues, but skeletal muscle tissue, heart, and smooth muscle are most affected. The most severely ill patients have reduced or absent GAA activity and usually die within the first year of life. Less severely ill patients may not be diagnosed until they reach adulthood. The incidence of Pompe disease is estimated at 1/40,000.1-5
Symptoms2
Pompe disease is classified as follows:
Infantile Pompe disease (IOPD):
- Patients who exhibit rapidly progressive disease characterized by prominent cardiomegaly, hepatomegaly, weakness and hypotonia and death due to cardiorespiratory failure in the first year. This represents the most severe end of the disease spectrum and is often referred to as classic infantile Pompe disease. Little to no detectable enzyme activity (<1%).
- Patients with the infantile variant form with slower progression and less severe cardiomyopathy but still presenting in the first year of life are classified as nonclassic infantile Pompe disease.
Late-onset Pompe disease (LOPD):
- Childhood, juvenile or muscular variant that is a heterogeneous group usually presenting later than infancy and typically not including severe cardiomyopathy.
- Adult-onset form characterized by a slowly progressive myopathy predominantly involving skeletal muscle that can present as late as the second to sixth decade of life.
References
-
Reuser AJ, Hirschhorn R, Kroos MA. Pompe Disease: Glycogen Storage Disease Type II, Acid α-Glucosidase (Acid Maltase) Deficiency. In: Valle DL, Antonarakis S, Ballabio A, Beaudet AL, Mitchell GA. eds. The Online Metabolic and Molecular Bases of Inherited Disease. McGraw Hill; 2019. Accessed December 04, 2023, https://ommbid.mhmedical.com/content.aspx?bookid=2709§ionid=225890450
-
Kishnani PS, Steiner RD, Bali D et al. Pompe disease diagnosis and management guideline. Genet Med. 2006;8(5):267-288
-
Kishnani PS, Goldenberg PC, DeArmey SL et al. Cross-reactive immunologic material status affects treatment outcomes in Pompe disease infants. Mol Genet Metab. Jan 2010;99(1):26-33
-
Kishnani PS, Steiner RD, Bali D et al. Pompe disease diagnosis and management guideline. J Pediatr 2006;148:671-676
-
American Association of Neuromuscular & Electrodiagnostic Medicine. Al-Lozi MT, Amato AA, Barohn RJ et al. Diagnostic criteria for late-onset (childhood and adult) Pompe disease. Muscle Nerve. 2009;40(1):149-160
-
Ausems MGEM, Verbiest J, Hermans MMP et al. Frequency of glycogen storage disease type II in The Netherlands: implications for diagnosis and genetic counselling. Eur J Hum Genet. 1999;7:713-716
-
Taglia A, Picillo E, D’Ambrosio P et al. Genetic counseling in Pompe disease. Acta Myologica. 2011;30:179-181
-
Byrne BJ, Kishnani PS, Caseet LE et al. Pompe disease: Design, methodology, and early findings from the Pompe Registry. Mol Genet Metab. 2011;103(1):1-11
-
Winkel LPF, Hagemans MLC, van Doorn PA, et al. The natural course of non-classic Pompe’s disease; a review of 225 published cases. J Neurol 2005; 252: 875-884





