Mucus plugs in Asthma, and the influence of Type 2 inflammation
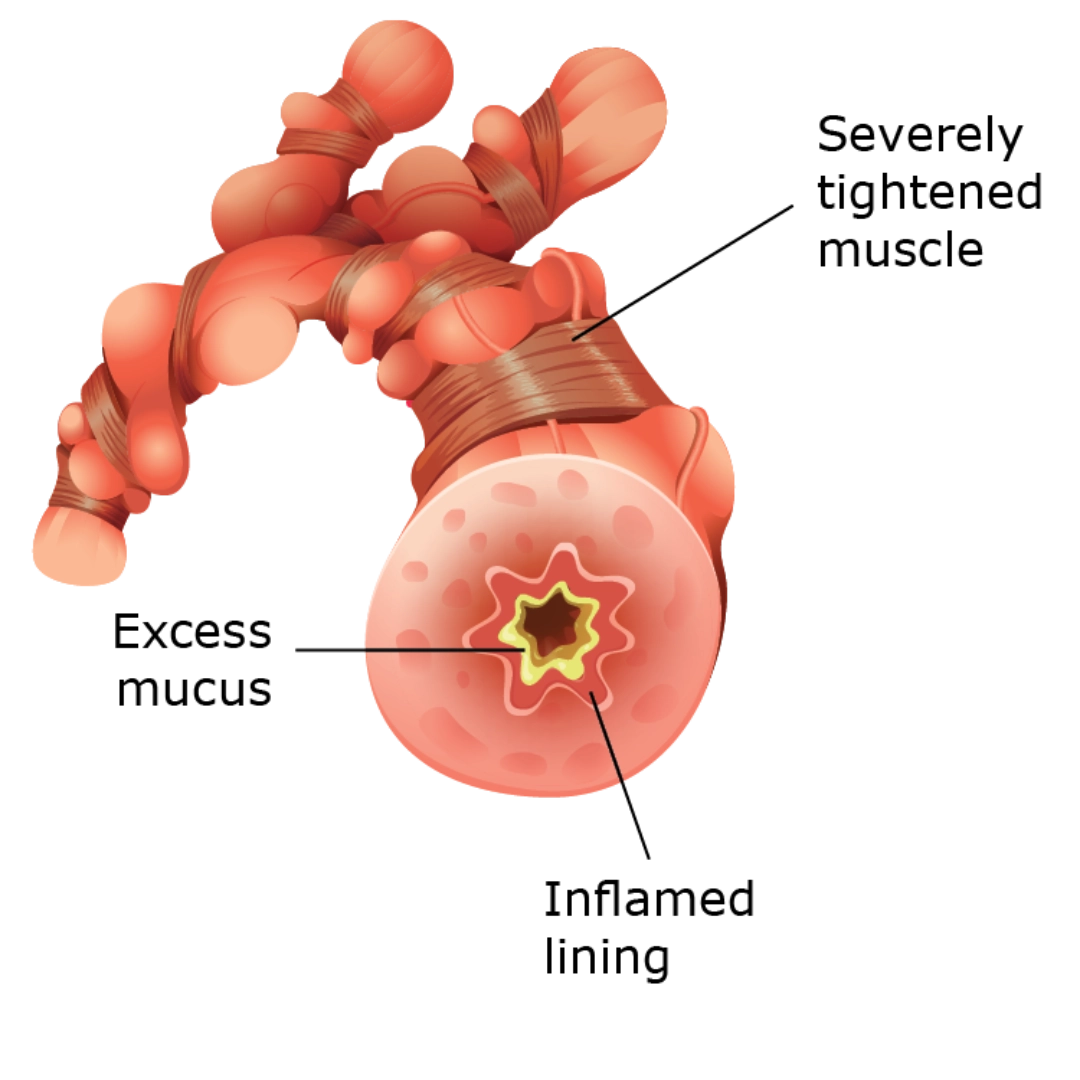
Mucus plugs are a critical yet often overlooked aspect of asthma that significantly contribute to airway obstruction and disease progression.1
Understanding the mechanisms behind their formation, particularly the role of type 2 inflammation and the cytokine IL-13, is essential for improving asthma management.1
- for maintaining airway health,
- trapping irritants,
- and facilitating gas exchange
Healthy mucus consists of approximately 97% water and a mixture of mucins, proteins, salts, and lipids, which must be well-regulated to ensure proper lung function.1
Type 2 inflammation and IL-13
Type 2 inflammation is characterized by the activation of T-helper 2 (Th2) cells and innate lymphoid cells (ILC2s), leading to the production of cytokines, particularly IL-4, IL-5, and IL-13.1
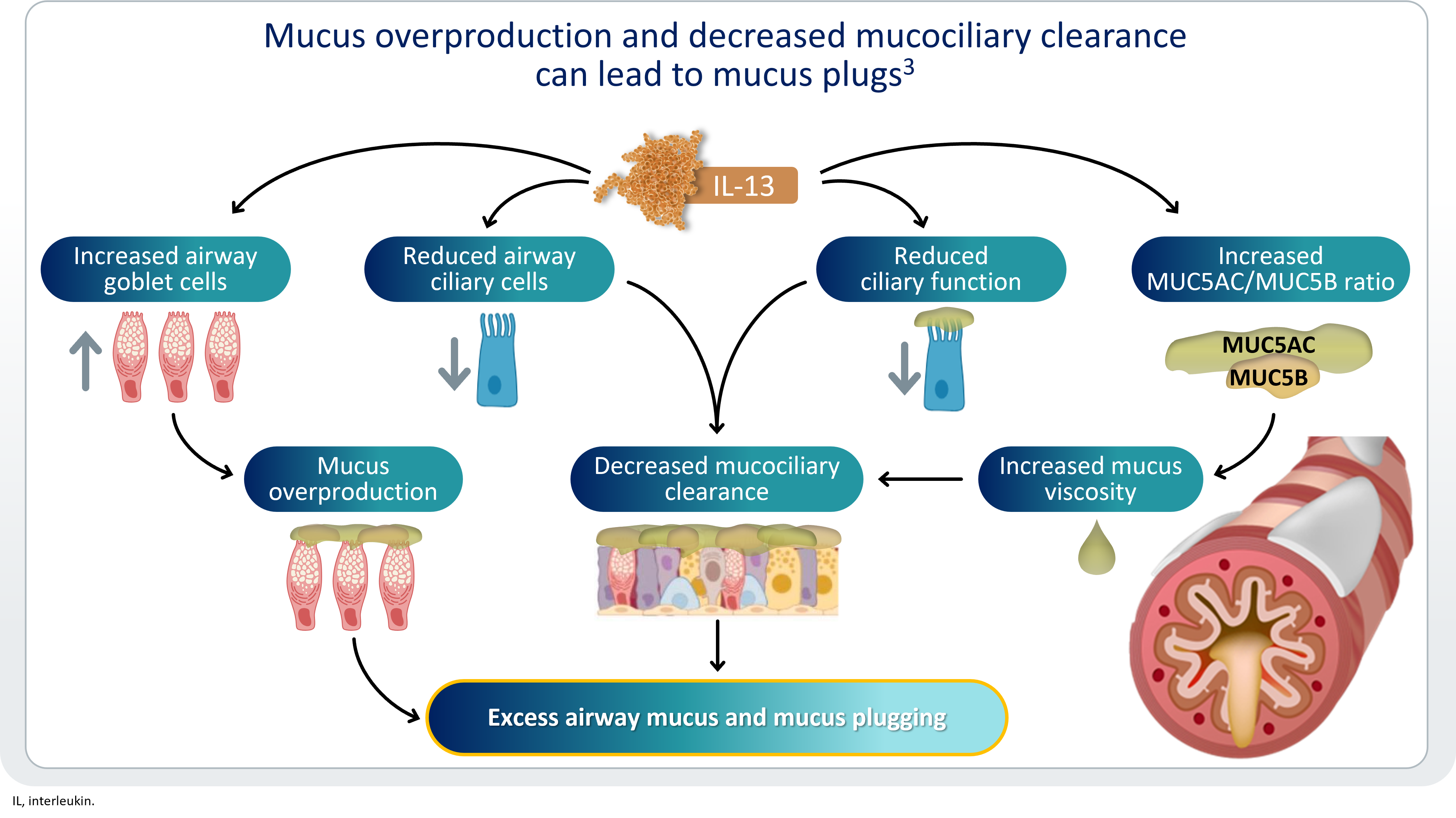
IL-13 is a key driver of mucus hypersecretion in asthma, significantly increasing the expression of MUC5AC, a mucin that contributes to mucus plug formation.1
IL-13 is mainly responsible for mucus overproduction and decreased mucociliary clearance1,2
Increased levels of MUC5AC lead to mucus plugs that are resistant to clearance, contributing to airway obstruction and exacerbations.1
In asthma, the ratio of MUC5AC to MUC5B is dysregulated, with MUC5AC being dramatically upregulated, particularly in eosinophilic asthma. This change results in mucus that is stickier and more tenacious.1
MUCUS PLUGGING IS A KEY COMPONENT OF REMODELING IN ASTHMA, LEADING TO FIXED OBSTRUCTION AND LUNG FUNCTION DECLINE3-5
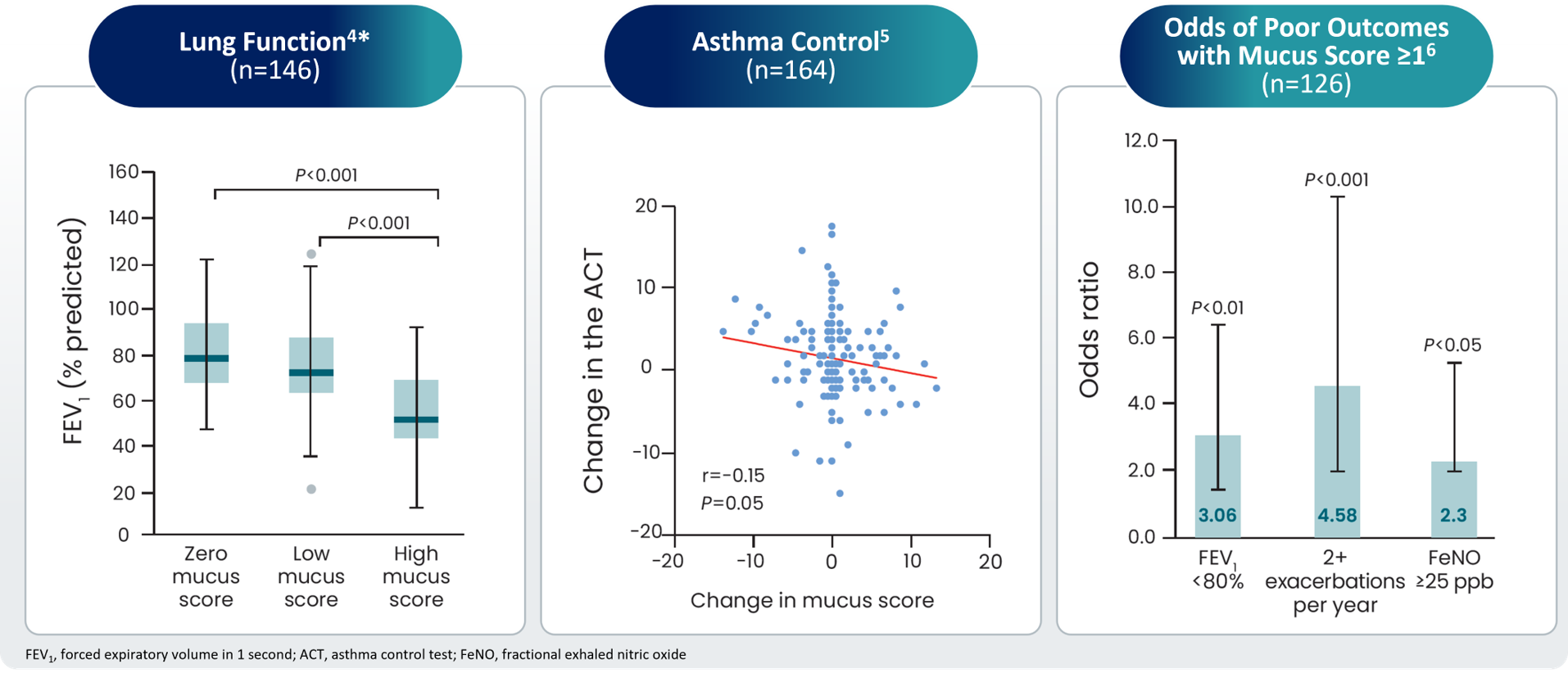
Presence of mucus plugs is associated with worsening clinical asthma outcomes6
Patients with high mucus scores have substantially2,6:
- increased IL-13 levels and eosinophil counts in sputum
- increased level of FeNO, another biomarker of type 2 inflammation
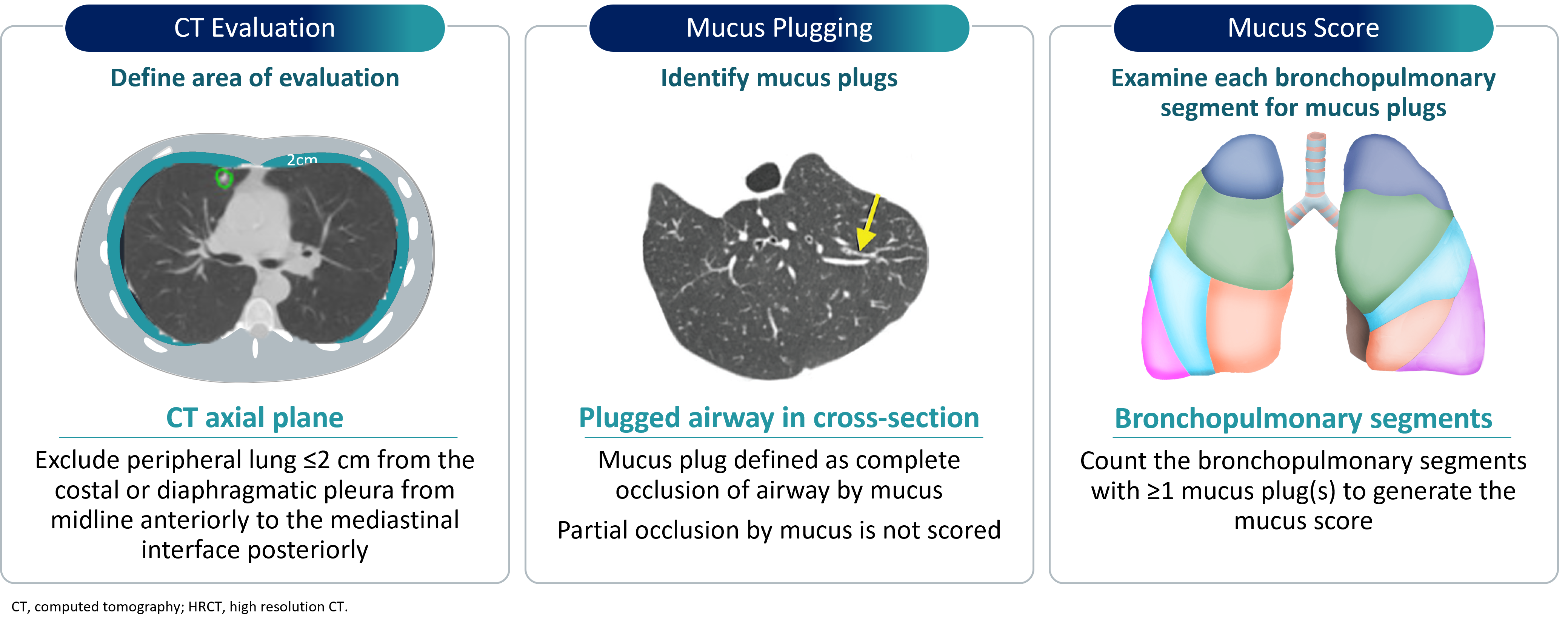
Segments of each lobe are examined for mucus plugs and given a score of 1 (present) or 0 (absent). Segment scores of each lobe are summed to generate a total mucus score ranging from 0-20.5
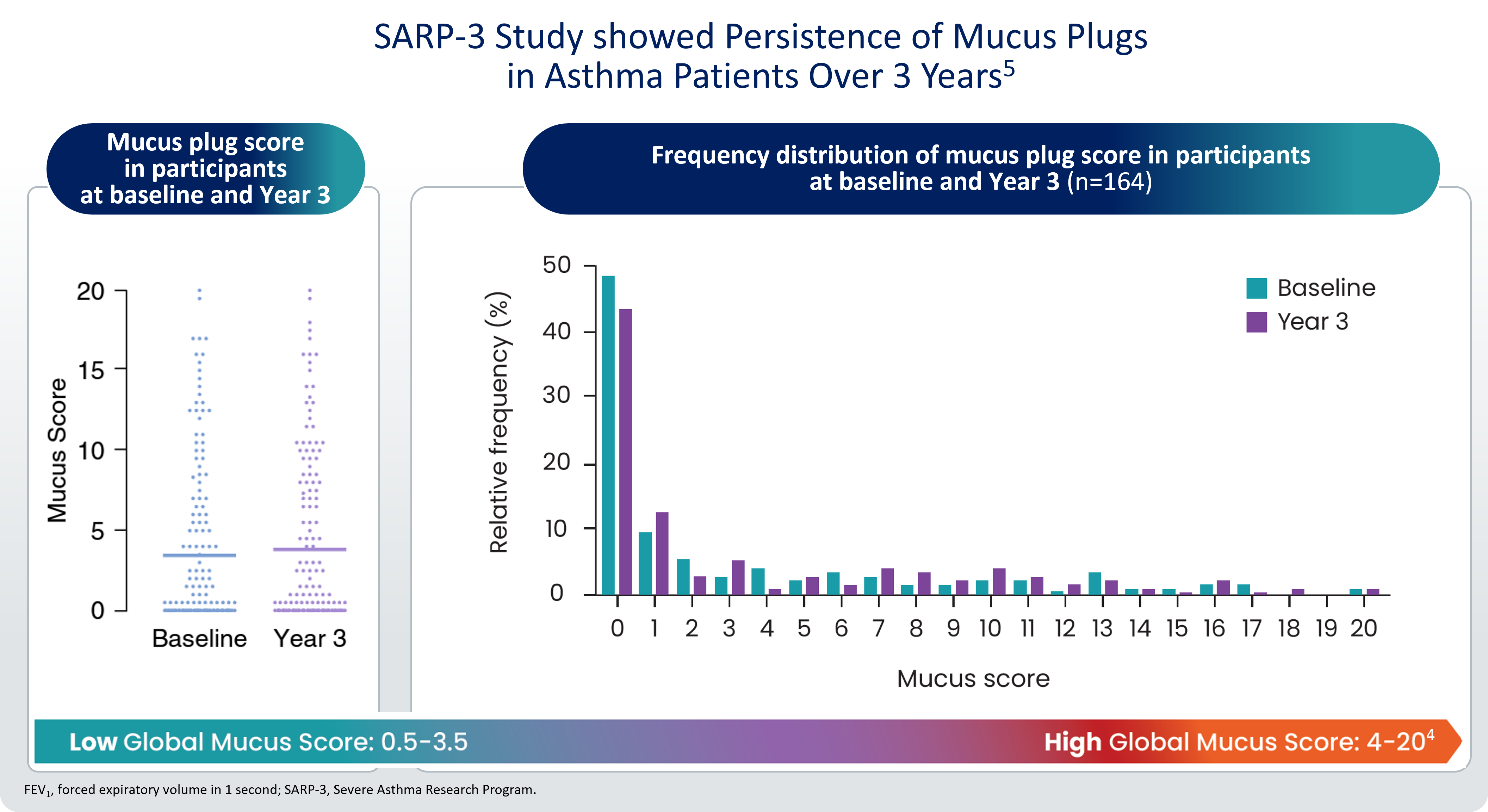
The change in mucus plug score from baseline to Year 3 was significantly negatively correlated with change in FEV1% predicted (P<0.001).5
Persistent mucus plugs are associated with chronic OCS use and greater symptom burden, measured by ACT3.5
To know more about mucus plugging
Republished with permission of American Society for Clinical Investigation, from Journal of Clinical Investigation, Dunican EM, Mucus plugs in patients with asthma linked to eosinophilia and airflow obstruction, Vol 128/No. 3, Copyright 2018; permission conveyed through Copyright Clearance Center, Inc. Reprinted from the American Journal of Respiratory and Critical Care Medicine, Tang M, et al, Mucus Plugs Persist in Asthma, and Changes in Mucus Plugs Associate with Changes in Airflow over Time, Vol 205/Issue 9,Copyright 2022, with permission from the American Thoracic Society.
*Data from 146 of the 658 adult patients with asthma enrolled in SARP. Of those included in SARP (n=658), 66% of patients met American Thoracic Society/European Respiratory Society criteria for severe asthma. Patients were non-smokers and were required to have evidence of bronchial hyperresponsiveness or reversible airflow obstruction.
ACT, Asthma Control Test; FeNO, fractional exhaled nitric oxide; FEV1, forced expiratory volume in 1 second; OCS, oral corticosteroid; SARP, Severe Asthma Research Program
-
Aegerter, H., et al. The Pathology of Asthma: What Is Obstructing Our View? Annual Review of Pathology: Mechanisms of Disease. Annu Rev Pathol. 2023 Jan 24:18:387-409.
-
Nakagome K, et al. Biomolecules. 2024;14(5):546.
-
Jesenak M, et al. Respir Med. 2023;218:107372.
-
Dunican EM, et al. J Clin Invest. 2018;128(3):997-1009.
-
Tang M, et al. Am J Respir Crit Care Med. 2022;205(9):1036-1045
-
Chan R, et al. J Allergy ClinImmunol Pract. 2023;11(1):195-199.e2