Why Choose Toujeo® (Insulin Glargine)
Quick Facts
- Once-daily basal insulin administration at any time of day, with a flexible administration window of 6 hours1
- Available in two prefilled pens: Toujeo SoloStar® and Toujeo DoubleStar®1
- Proven efficacy and safety profile demonstrated in head-to-head clinical trials2,3
- Flexible dosing option with individualized dose adjustment for type 2 diabetes management1
Flexible Once-Daily Dosing
Toujeo offers flexible once-daily dosing with two prefilled pen options1:
References : A. TOUJEO® Summary of product characteristics (2024). B. Becker RH, et al. Diabetes Care 2015;38(4):637–643. C. Bergenstal et al. Diabetes Care. 2017;40(4):554-560. D. Bailey TS, et al. Diabetes Metab. 2018;44:15–21. E. Riddle MC, et al. Diabetes Technol Ther. 2016;18:252–7. F. Matsuhisa M et al., Diabetes, Obesity and Metabolism 18: 375-383, 2016. G. Ritzel R et al. Diabetes Obes Metab. 2015 Sep;17(9):859-67.
Key Benefits
- Allows for personalized dosing through individual dose adjustments1
- Supports patient adherence with once-daily administration1,2
- Provides options for different insulin requirements1
Proven Efficacy and Safety
BRIGHT Study Overview
The Bright study demonstrated similar efficacy and safety of Toujeo® (Glargine 300, n=466) compared to degludec 100 (n=463) in type 2 diabetes patients who had not previously received basal insulin.1
Key Observations
- Similar glycaemic control for HbA1c demonstrating non-inferiority of Toujeo compared to degludec (p<0.0001 for non onferiority of Toujeo)2,3
- Lower incidence of hypoglycemia during the initial titration phase (0-12 weeks) with Gla-300 vs IDeg-1004
- 0.49 gla-300 vs. 0.86 ideg-100 ER* (events per patient-year)
- p=0,038 ¥
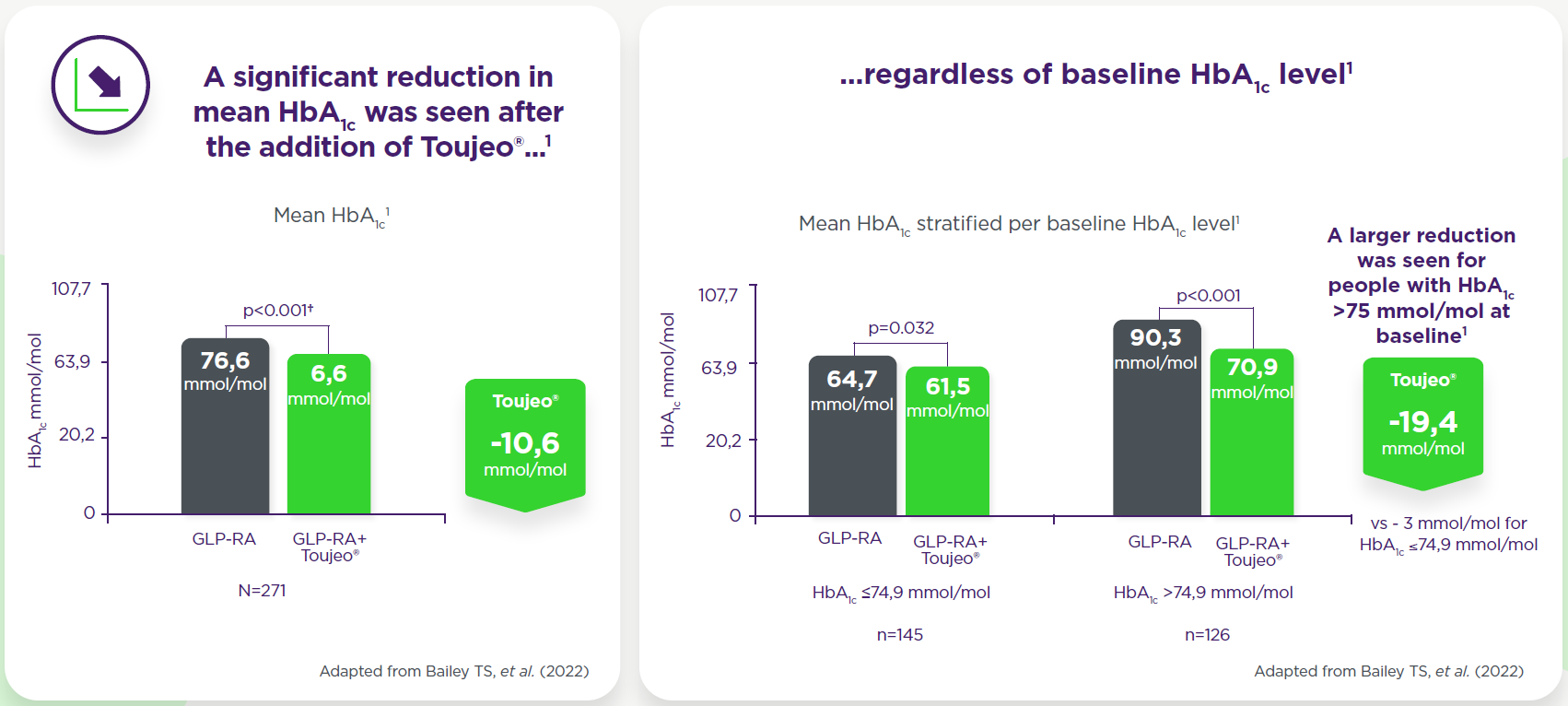
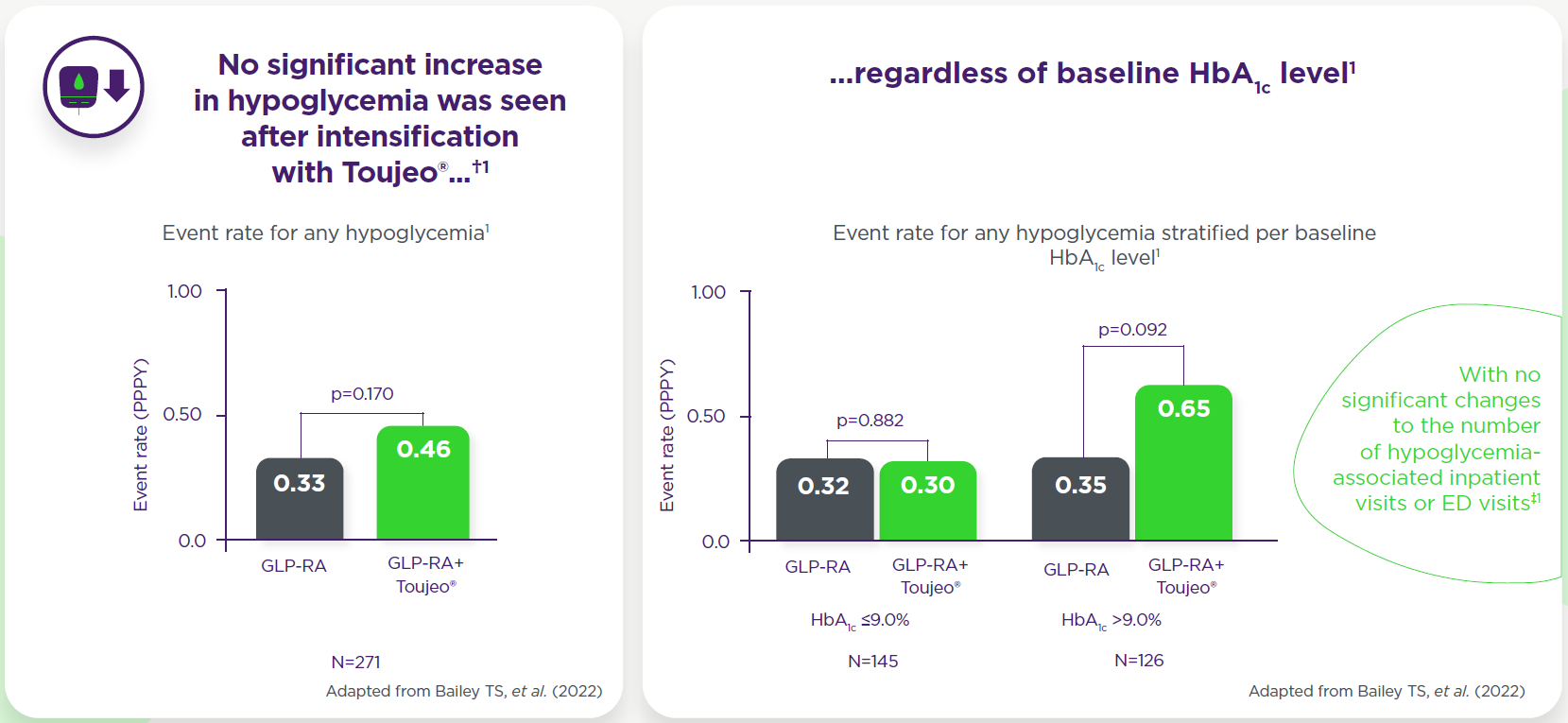
Benefits When Adding Toujeo to GLP-1 RA Therapy
EASD and ADA recommend the addition of basal insulin for people with T2DM who do not achieve glycemic goals on a GLP-1 RA-based regimen.*6,7
The DELIVER-G study explores the real-world outcomes of adding Insulin Glargine 300 U/mL (Gla-300) to GLP-1 receptor agonist (GLP-1RA) therapy in people with type 2 diabetes (PWD2)5 †1
Key Observations
1. Significant improvement in glycemic control5
2. No significant increase in hypoglycemia5
3. Stable weight and body mass index (BMI)5

Weight/BMI remained stable, but proportion of patients with BMI ≥35 kg/m² increased by 3.9% (51.5% to 55.4%; p=0.046)5
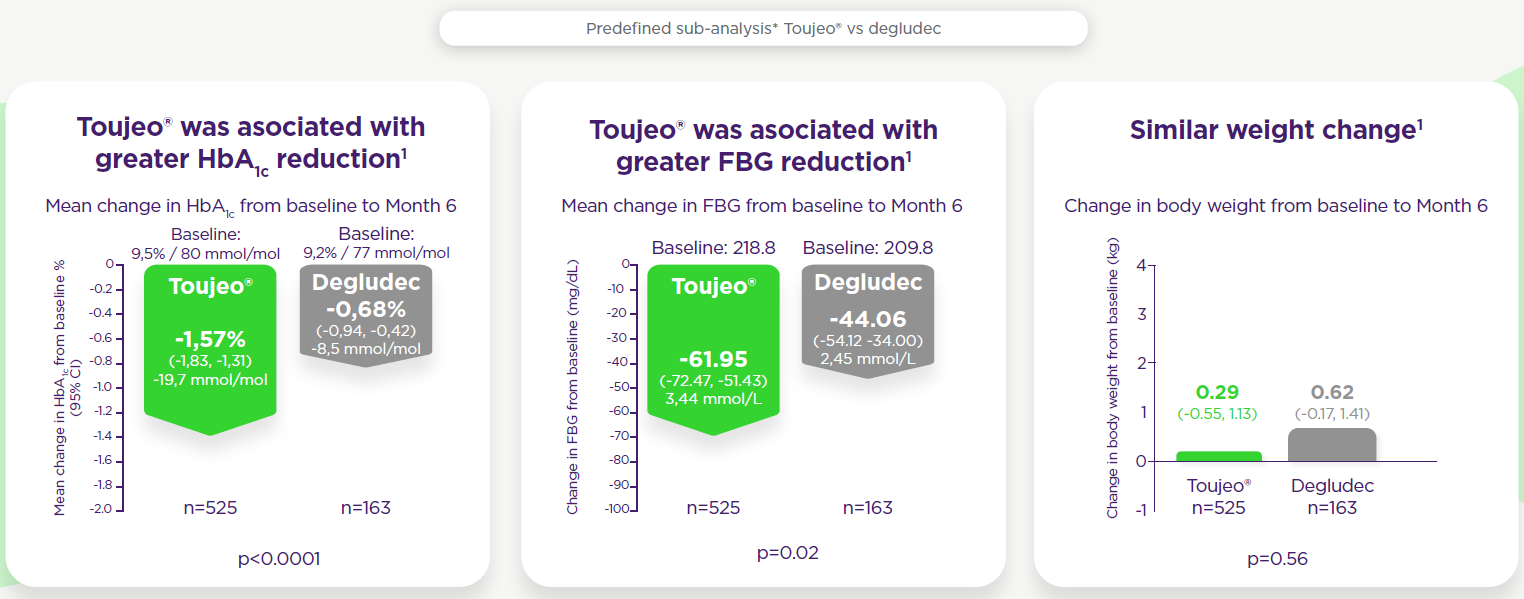
Switching to or adding on basal insulin to GLP-1 RA therapy
EASD and ADA recommend the addition of basal insulin for people with T2DM who do not achieve glycemic goals on a GLP-1 RA-based regimen.*6,7
RESTORE-G: RESTORE-G was a real-world analysis in insulin-naïve adults with type 2 diabetes mellitus (T2DM) previously treated with GLP-1 receptor agonists (GLP-1 RA) ± oral antidiabetic drugs (OADs), examining therapy intensification through three approaches involving basal insulin analogues8:
- Starting basal insulin and discontinuing GLP-1 RA
- Adding basal insulin to ongoing GLP-1 RA
- Initiating a FRC product and discontinuing current GLP-1 RA†1.
Key Observations
Primary Endpoint Results
- ~40% of people with T2DM on GLP-1 RA required intensification with basal insulin after a median of ~2 years.8, ‡1
- Following intensification with basal insulin
- Significant reduction in HbA1c was observed§
- No severe hypoglycemia was recorded.¥8
In patients who switched to a second-generation BI (either gla-300 or Deg-100) Toujeo was associated with greater HbA1c and FBG reductions, and similar weight change vs degludec, in people with T2DM switching from GLP-1 RA therapy to basal insulin.8,9
Greater HbA1c reduction with Toujeo® vs degludec was also seen in the propensity score matched sensitivity analysis (p=0.02)†‡1
Key Observations
- Second Generation vs First Generation Basal Insulins: Second-generation basal insulins were more effective in improving glycemic control when added to or replacing therapy in patients already on GLP-1 receptor agonists (GLP-1 RA).8,9
- Glargine 300 (Toujeo) vs. Degludec 100: Among second-generation options, in patients who switched Glargine 300 (Toujeo) led to greater HbA1c reduction compared to Degludec 100 U/mL.8,9.
- Free vs. Fixed Combinations: Both free and fixed combinations of GLP-1 RA and basal insulin were effective. The choice should be tailored to individual patient needs and preferences.8,9
Study population were insulin naive. No specific safety concerns were reported. Overall, 202 (43.7%) and 221 (47.8%) of participants in the Toujeo® and degludec treatment groups, respectively, reported adverse events during the 24-week study period.1
Week 12 ITT population: Toujeo®, n=448; degludec, n=445.3 Week 24 ITT population: Toujeo®, n=462; degludec, n=462.1
† Comparable incidence and rates of hypoglycemia in the maintenance period (13–24 weeks) and full 24-week study period, were demonstrated.1
* LSM change in HbA1c from baseline to Week 12 with Toujeo® was -1.37% vs -1.39% with degludec. LSM difference: 0.02% (95% CI: -0.08, 0.12). The non-inferiority margin was 0.3%.1, 2
** Figure 2 – Hypoglycemia at any time of day (24 h) (A) or during the nocturnal period (0000-0559 h) (B), safety population. Nominal P values are provided, Rosenstock J, et al. Diabetes Care. 2018;6
‡Anytime (24 h) confirmed hypoglycemia (≤70 and <54 mg/dL) and nocturnal (00:00–05:59 h) confirmed hypoglycemia (≤70 mg/dL).1
§Events per patient-year: Toujeo®, 0.49; degludec, 0.86.1
¥Nominal p-value.1
CI, confidence interval; degludec, insulin degludec 100 U/mL; HbA1c, hemoglobin A1c; ITT, intent-to-treat; LSM, least squares mean; RR, rate ratio; T2DM, type 2 diabetes mellitus, ER, event rate.
* Pre-post, retrospective, cohort study. Data relative to adults with T2DM with at least 1 prescription of GLP-1 RA were extracted from electronic medical records (i.e.SmartDigitalClinic - METEDA). Index dates ranged from January 2011 to September 2021.1
† 39.7% of insulin-naïve people with T2DM changing their therapy discontinued/modified the GLP-1 RA treatment, switching to BI or FRC or added on BI to ongoing GLP-1 RA treatment.1 ADA, American Diabetes Association; BI, basal insulin; CI, confidence interval; EAD, European Association for the Study of Diabetes; FRC, fixed-ratio combination; GLP-1 RA, glucagon-like peptide-1 receptor agonist; OAD, oral antidiabetic drug; T2DM, type 2 diabetes mellitus.
* This predefined sub-analysis is propensity score adjusted taking into account baseline differences. All models were adjusted for propensity scores estimated taking into account age, gender, diabetes duration, baseline HbA1c, BMI, FBG, basal insulin dose, eGFR <60 mL/min*1.73m2, history of diabetes complication, concomitant glucose lowering treatments. Rates of hypoglycemia were not assessed in this comparative sub-analysis.1
† Variables included in the PS matching model were the same used for the PS adjustments. A 5-to-1 greedy matching algorithm was used to identify a unique matched control for each Toujeo® patient according to the PS. Adequacy of balance for the covariates in the matched sample was assessed via standardized mean difference between the two groups, considering differences <0.10 (absolute values) as good balance. Longitudinal models were adjusted for unbalanced variables after PS matching.1
‡ Change in HbA1c from baseline to Month 6 (95% CI) in the propensity score matched analysis: -1.34 (95% CI: -1.67; -1.01) with Toujeo® vs -0.78 (95% CI: -1.12; -0.44) with degludec, estimated mean difference -0.55% (95% CI: -1.02, -0.08); p=0.02.1
BMI, body mass index; CI, confidence interval; eGFR, estimated glomerular filtration rate; FBG, fasting blood glucose; GLP-1 RA, glucagon-like peptide-1 receptor agonist; HbA1c, hemoglobin A1c; OAD, oral antidiabetic drug; PS, propensity score; T2DM, type 2 diabetes mellitus.
Insulin-naïve adult patients (N=271) with T2DM receiving GLP-1 RA therapy ± OAD(s) that was subsequently intensified by adding Toujeo®. A total of 156 (57,6%) patients received daily GLP-1 RA and 115 (42,2%) received weekly GLP-1 RA before treatment intensification; 250 (92,3%) patients were receiving at least one OAD prior to intensification with Toujeo® (the mean number of OADs was two).
*Data were extracted from a US electronic medical record data source (IBM® Explorys). Patients selected for inclusion had ≥12 months’ pre-Toujeo® data and ≥6 months of follow-up data.
**Paired Student’s t-test. Change in HbA1c between baseline and follow-up was assessed using the last value recorded within the 3- to 9-month period following intensification with Toujeo®.
†Identified by ICD-9 or ICD-10 codes, or a blood glucose recording ≤70 mmol/L, or the number of hypoglycaemic events in the 6-month baseline period vs the 6-month follow-up period. Incidence of any hypoglycaemia pre- and post-intensification with Toujeo® was 8,49% and 9,59%, respectively (p=0,513). Paired Student’s t-test.
‡One hypoglycaemia-associated inpatient visit was recorded during the baseline period and none during the follow-up period after intensification with Toujeo®; no hypoglycaemia-associated ED visits were recorded during the baseline period and one during the follow-up period. Incidence of any (8,49% vs 9,59%, p=0,513), and inpatient/ED-associated hypoglycaemia (0,37% vs 0,74%, p=1,000), as well as event rates of any (0,33 vs 0,46 PPPY, p=0,170) and inpatient/ED-associated hypoglycaemia (0,01 vs 0,04 PPPY, p=0,466) were similar before and after addition of Toujeo®. When analysed by baseline GLP-1 RA regimen, incidence of hypoglycaemia increased from baseline to follow-up (3,9% to 8,3%, p=0,02; event rate 0,21 to 0,44 PPPY, p=0,017) for those on daily GLP-1RAs. No significant change was observed for those on weekly GLP-1 RAs.
-
Toujeo® Summary of Product Characteristics
-
Rosenstock J, et al. Diabetes Care. 2018;41:2147-2154
-
Cheng A. et al. Diabetes Obes Metab. 2020;22:346–354.
-
ClinicalTrials.gov. Efficacy and safety of Toujeo® versus Tresiba® in insulin-naïve patients with type 2 diabetes mellitus inadequately controlled with oral antihyperglycemic drug(s) ± GLP-1 receptor agonist (BRIGHT) [NCT02738151]. Available at: https://clinicaltrials.gov/ct2/show/NCT02738151 (Accessed May 2023).
-
Bailey TS, et al. Real-world outcomes of addition of insulin glargine 300 U/mL (Gla-300) to GLP-1 RA therapy in people with type 2 diabetes: The DELIVER-G study. Diabetes Obes Metab. 2022;doi: 10.1111/dom.14739.
-
Davies MJ, et al. Diabetes Care. 2018;41:2669–701;
-
American Diabetes Association. Diabetes Care. 2024;47 (Suppl 1): S158-S178;
-
Candido R, et al. Nutr Metab Cardiovasc Dis. 2023;33(11):2294-2305.
-
Davies MJ, et al. Diabetes Care. 2022;45:2753–2786.
TOUJEO® (insulin glargine 300 units/ml) – Abbreviated Prescribing Information
NAME AND PRESENTATION: Toujeo® 300 units/ml SoloStar, solution for injection in a prefilled pen. Toujeo® 300 units/ml DoubleStar, solution for injection in a pre-filled pen. 1 ml of solution contains 300 units of insulin glargine. Each SoloStar prefilled pen contains 1,5 ml of solution for injection (equivalent to 450 units). Each DoubleStar pen contains 3 ml of solution for injection (equivalent to 900 units). THERAPEUTIC INDICATIONS: Treatment of diabetes mellitus in adults, adolescents and children from the age of 6 years. POSOLOGY AND METHOD OF ADMINISTRATION*: Toujeo® is a basal insulin for once-daily administration at any time of the day, preferably at the same time every day. When needed, patients can administer Toujeo® up to 3 hours before or after their usually time of administration. The dose regimen (dose and timing) should be adjusted according to individual response. In type 1 diabetes mellitus, Toujeo® is to be used once-daily and must be combined with short-/rapid-action insulin to cover mealtime insulin requirements. In patients with type 2 diabetes mellitus, the recommended daily starting dose is 0.2 units/kg. Toujeo® can also be given together with other anti-hyperglycaemic medicinal products. Switch: When switching from insulin glargine 100 units/ml to Toujeo®, this can be done on a unit-to-unit basis. When switching from a treatment regimen with an intermediate or long-action insulin to a regimen with Toujeo®, a change of the dose of the basal insulin may be required and the concomitant anti-hyperglycaemic treatment may need to be adjusted. Close metabolic monitoring is recommended during the switch and in the initial weeks thereafter. For switch details see full SmPC. Special populations: Toujeo® can be used in elderly people, renal and hepatic impaired patients and adolescents and children ≥6 years. Renal impairment & hepatic impairment: insulin requirements may be diminished. Elderly: progressive deterioration of a renal function may lead to a steady decrease in insulin requirements. Children: Toujeo® can be used in in adolescents and children based on the same principles as adult patients. When switching to Toujeo®, dose reduction on basal and bolus insulins needs to be considered on an individual basis to minimize risk of hypoglycaemia. Safety and efficacy in children below 6 years have not been established, no data are available. Method of administration: For subcutaneous use only. Rotate injection sites to reduce the risk of lipodystrophy and cutaneous amyloidosis. Toujeo® must not be administered intravenously or in insulin infusion pumps. The Toujeo® SoloStar and Toujeo® DoubleStar pre-filled pens have been specifically designed for Toujeo® and no dose re-calculation is required for either pen. When changing from Toujeo® SoloStar to Toujeo® DoubleStar, if the patient’s previous dose was an odd number (e.g. 23 units) then the dose must be increased or decreased by 1 unit (e.g. 24 or 22 units). Toujeo® DoubleStar prefilled pen is recommended for patients requiring at least 20 units per day. Toujeo® must not be drawn from the cartridge of the Toujeo® SoloStar pre-filled pen or Toujeo® DoubleStar pre-filled pen into a syringe or severe overdose can result. For administration details see full SmPC. CONTRAINDICATIONS*: Hypersensitivity to the active substance or to any of the excipients listed in the full SmPC. SPECIAL WARNINGS AND PRECAUTIONS FOR USE*: Record name and batch number of administered product to improve traceability of biological medicinal products. Toujeo® is not the insulin of choice for the treatment of diabetic ketoacidosis. Instruct patients to continuously rotate injection site to reduce risk of lipodystrophy and cutaneous amyloidosis; delayed insulin absorption and worsened glycaemic control may occur after injection at affected sites. Sudden change in injection site to unaffected area has resulted in hyperglycaemica; blood glucose monitoring is recommended after changing injection site and dose adjustment of antidiabetic medications may be considered. The prolonged effect of insulin glargine may delay recovery from hypoglycaemia. Insulin glargine 100 units/ml and Toujeo® are not bioequivalent and are not interchangeable and switching may result in the need for a change in dose and should only be done under strict medical supervision. Switching patients between other insulins and Toujeo® should be done under strict medical supervision and may result in the need for a change in dose. Intercurrent illness requires intensified metabolic monitoring. In rare cases the presence of insulin antibodies may necessitate adjustment of insulin dose. If pioglitazone is used in combination with insulin, especially in patients with risk factors for development of cardiac heart failure, patients should be observed for signs and symptoms of heart failure, weight gain and oedema. Pioglitazone should be discontinued if any deterioration in cardiac symptoms occurs. For further details on special warnings and precautions for use see full SmPC. DRUG INTERACTIONS*: Substances that may enhance or reduce the blood glucose-lowering activity and increase susceptibility to hypoglycaemia are detailed in the full SmPC. PREGNANCY AND LACTATION*: There is no clinical experience with use of Toujeo® in pregnant women. For insulin glargine no clinical data on exposed pregnancies from controlled clinical studies are available. A large amount of data on pregnant women indicate no specific adverse effects on pregnancy and no specific malformative nor feto/neonatal toxicity of insulin glargine. The use of Toujeo® may be considered during pregnancy if clinically needed. It is unknown whether insulin glargine is excreted in human milk. No metabolic effects on breast-fed newborn/infant are anticipated as insulin glargine is digested into amino acids in the gastrointestinal tract. EFFECTS ON ABILITY TO DRIVE*: Patient’s ability to concentrate and react may be impaired as a result of hypoglycaemia or hyperglycaemia or, for example, as a result of visual impairment. Patients should be advised to take precautions to avoid hypoglycaemia whilst driving. UNDESIRABLE EFFECTS*: Very common: Hypoglycemia. Hypoglycaemia may occur if the insulin dose is too high in relation to the insulin requirement. Common: Lipohypertrophy; injection site reactions. For full list of undesirable effects consult the full SmPC. Clinical study safety data not available for children <6 years. OVERDOSAGE*: Mild episodes of hypoglycaemia can usually be treated with oral carbohydrates. More severe episodes may be treated with intramuscular/subcutaneous glucagon or concentrated intravenous glucose. PHARMACOLOGICAL PROPERTIES: ATC Code: A10A E04. MARKETING AUTHORIZATION HOLDER: Sanofi-Aventis Deutschland GmbH, D 65926 Frankfurt am Main, Germany. LEGAL CATEGORY: Medicinal product subject to medical prescription. DATE OF LAST REVIEW: August 2024
*Abbreviated Prescribing information based on the EU SmPC as of Nov 2023.
Before prescribing the product always refer to your full local prescribing information as this information may vey from country to country.
For local details, please refer to below information.
Sweden: Rx, (F), A10AE04. Toujeo is reimbursed for all patients with type 1-diabetes and for patients with type 2-diabetes where other insulin treatments are not sufficient to reach the treatment target because of repeated hypoglycaemic events. For further information, and also information concerning price and packaging, see www.fass.se. In Sweden Toujeo is provided by Sanofi AB, Box 30052, 104 25 Stockholm, Tel: +46 8 634 50 00, www.sanofi.se. For questions on our medicinal products, please contact: infoavd@sanofi.com.